|
|
 |
| |
|
|
 |
Introduction¡G |
| |
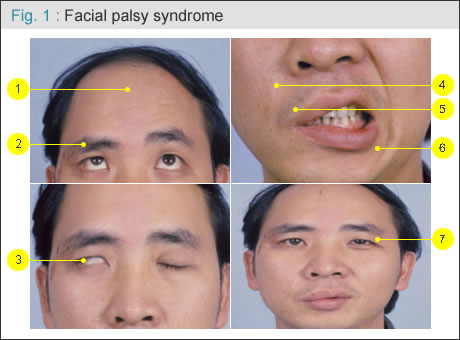
Facial palsy (or paralysis) has a devastating psychological impact on the affected individual. The facial nerve travels from the cortex, brainstem, cerebellopontine angle (intracranial portion) to temporal bone (internal auditory canal, Fallopian canal, stylomastoid foramen ) and to the facial muscles (extracranial portion). Any lesion during its pathway can cause facial nerve injury and palsy, including congenital, trauma, tumor surgery, infection, or idiopathic (Bell¡¦s palsy). Patient will lose not only function of the mouth and eyelid (can not tightly close the eye and mouth, or making teeth expose when smiling), but also lose ability to form facial expression. With palsy, you might see patient lose face dynamic wrinkles (forehead or nasolabial fold), lagophthalmos (eye can not close tightly), easy tearing, drooling, lower eyebrow etc on the affected side, causing facial expression with asymmetry. There is no smiling at all on the affected side. When smiling, all lip will move to the intact side. Compensatory small eye of the intact side of eye will also be seen. All emotions (happiness, sorrow, joy, surprise, crying etc) show the same look on the affected side without any animation(Fig. 1 ). . |
 |
Management of facial paralysis depends upon the cause, including medical and surgical management. With idiopathic facial palsy (Bell¡¦s palsy) it is most treated medically. Neurosurgeons will take care of the intracranial portion. ENT surgeons care of the temporal facial canal. As plastic surgeons, we are primarily concerned with the extratemporal portion. Surgical procedures to restore facial function include:
Direct end-to-end coaptation: with a sharp, clean division, the severed nerve is repaired immediately under microscopic view, giving the best result.
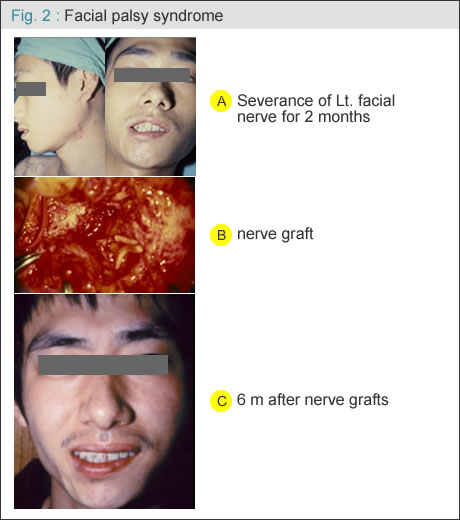
nerve graft: when nerve gap occurs due to nerve retracted or nerve segmental deficit by trauma or tumor resection, interposition of nerve graft is required( Fig. 2 A-C ).
|
 |
Nerve transfer: using hypoglossal or spinal accessory nerve or contralateral facial nerve transfer to the distal facial nerve for reinnervation as a one stage reconstruction in the early stage.
Asynchronous or weak reanimation limits its application.
Local muscle transfer: temporal muscle or masseter muscle transfer for part eye or mouth restoration. Asynchronous or weak reanimation limits its application.
Free muscle transplantation: for a long-standing facial palsy (over one year ), a classic two-stage procedure is preferred by most plastic surgeons:
Stage 1: cross-face nerve graft: a short nerve graft (10-15cm) harvested from leg through two small incisions.
6-9 months later
Stage 2: functioning free muscle transplantation: the muscle is usually harvested from the opposite thigh, gracilis muscle
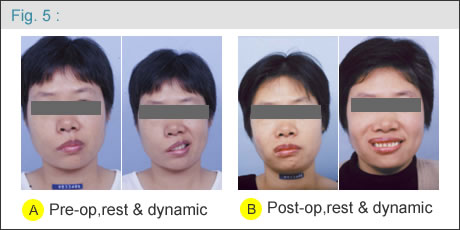
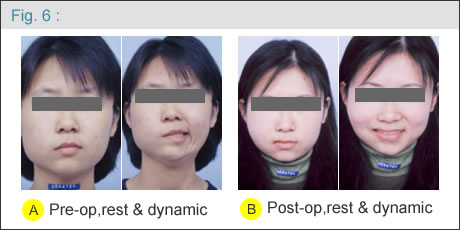
Between 1986 and 2006, more than 250 patients with facial palsy were treated with the classic two-stage procedure at Chang Gung Memorial Hospital, Taipei-Linkou, by the same surgeon (DCC Chuang). The results are promising ( Figure 4, 5, 6 ) and the treatment is continuous. |
 |
 |
 |
| |
|
 |
Relative articles: |
| |
| 1. |
Chuang CC, Cheng MH and Schrag C: A modified technique for rapid restoration of facial paralysis- short cross-face nerve graft, short waiting period, and free muscle transplantation. Plast Reconstr Surg (ROC) 15(2): 105-115, 2006 |
| 2. |
Chuang DCC, Mardini S, Lin SH, and Chen HC: Free proximal gracilis muscle and its skin paddle compound flap transplantation for complex facial paralysis. Plast Reconstr Surg 113(1): 126-32, 2004 |
| 3. |
Chuang DCC. Reanimating the paralyzed face after head and neck tumor excision. Seminars in Plastic Surgery 17(3): 331-40, 2003 |
| 4. |
Chuang DCC. Technique evolution for facial paralysis reconstruction using functioning free muscle transplantation- experience of Chang Gung Memorial Hospital. |
| 5. |
Clin Plastic Surg 29: 449-459, 2002 |
|
|
| |
|
|
|
|
|
 |

