|
|
 |
| |
|
|
 |
IntroductionˇG |
| |
Close traction injuries of the brachial plexus are always crippling injuries. It involves usually a plexus of nerves in a complicated anatomic arrangement. Extensive and various nature of the injury, long microneurosurgical operation, long regeneration period demanding long follow-up, long rehabilitation time and different palliative surgeries for sequelae deformities et cetera will always challenge and exhaust surgeons. Management of adult BPI should have (1) knowledge of anatomical arrangement, (2) pathophysiology considerations, ( 3 ) preoperative evaluation and diagnosis, (4) surgical technique, (5) postoperative management (6) rehabilitation and regular patientˇ¦s follow-up, ( 7 ) surgical treatment of sequelae deformities, and finally (8) understanding which factor will influence its results. |
| |
|
 |
Anatomy: |
| |
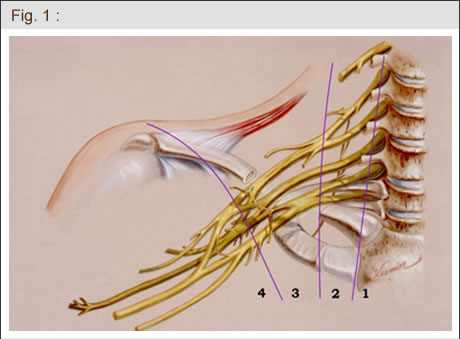
The brachial plexus is formed by the anterior primary rami of the lower cervical ( C5-C8) and the first thoracic ( T1 ) spinal nerves, which give motor innervation to muscles of the shoulder including all anterior and posterior chest muscles related to glenohumeral joint movement, muscles of the entire upper limb (extrinsic and intrinsic muscles ) and sensory innervation of the entire upper limb, except the skin on some part of the medial aspect of upper arm. BPI can be classified lesions into four levels: (1)preganglionic root lesions; (2) postganglionic spinal nerve lesions; (3) pre- and retroclavicular lesions ( trunks and divisions), and (4) infraclavicular brachial plexus lesions (cord and terminal branches) ( Fig 1 ). |
| |
 |
| |
Once injured, it will cause various motor and sensory disturbances of the upper limb based on level of injury. The majority of closed BPI in our adults population are preganglioinc root injury ( 73% ). There may be single or multiple root injuries. Differentiation between preganglionic root and postganglionic spinal nerve lesions is very important with respect to surgical procedure and predicting prognosis. |
| |
|
 |
Etiology: |
| |
Closed traction injuries are the most common brachial plexus injuries seen in the traumatized adult patients. In Taiwan, 70% victims are caused by motorcycle accident.
Diagnosis : Although accurate assessment of the extent and severity of the brachial plexus damages in closed BPI is very difficult, clinical evaluation is still an essential and most important step in establishing the diagnosis of type, degree and site of injury, and determining the treatment and prognosis. Diagnosis information includes the present illness, past history, motor and sensory examination, Tinelˇ¦s sign, pain character, Hornerˇ¦s syndrome, vascular lesions, mobility of diaphragm, and ancillary investigations such as plain X-ray, other imaging studies (computerized tomography, myelography, MRI), and EMG..
|
| |
|
 |
Treatment : |
| |
In an open injury in the neck region by knife or other sharp objects, causing significant motor and sensory deficits, transection (or disruption) of brachial plexus is highly suspected. An immediate or few days after trauma is indicated. However, closed traction injuries are the most common brachial plexus injuries seen in traumatized adult patients. Management of these patients can be considered in six stages: Stage 1: Stabilization stage ( the first month): including stabilization of vital signs, bone fracture or joint dislocation. Stage 2: Diagnostic stage ( the second month): including clinical examination and investigations to establish the diagnosis of the lesion condition; start physiotheraphy to prevent soft tissue swelling, joint stiffness, and slow muscle atrophy by electric stimulation; and psychologic education before surgery. Stage 3: Surgery ( the 3rd to 5th month ): If the patient fails to show a return of function at 3 months, surgical intervention is indicated. If the injury is not a high-speed energy such as bike accident or rolling door accident, the period of observation can be prolonged until 5 months. Nerve transfer or nerve grafts within 5 months seems no big difference in results of our series. Stage 4: Rehabilitation stage; requiring at least 3 years. Stage 5: Late reconstructive stage: usually performed during the third and fourth year postoperatively, including tendon transfer, functioning free muscle transplantation, wrist arthrodesis, orthodesis etc . Stage 6: Destination stage: fifth year postoperatively. |
| |
|
 |
Surgical methods : |
| |
The available techniques in brachial plexus surgery include ( 1 ) neurolysis, (2) direct nerve repair, (3) nerve repair with nerve grafts (free or vascularized ), (4) nerve transfer, and (5) functioning free muscle transplantation. |
| |
|
 |
Surgical outcomes : |
| |
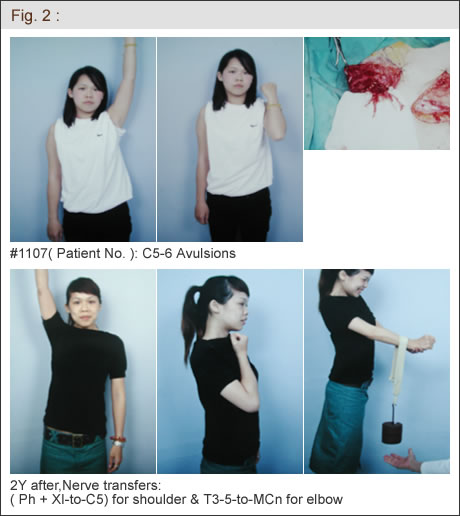
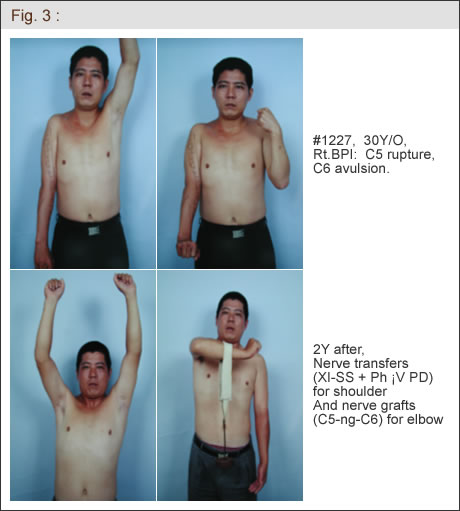
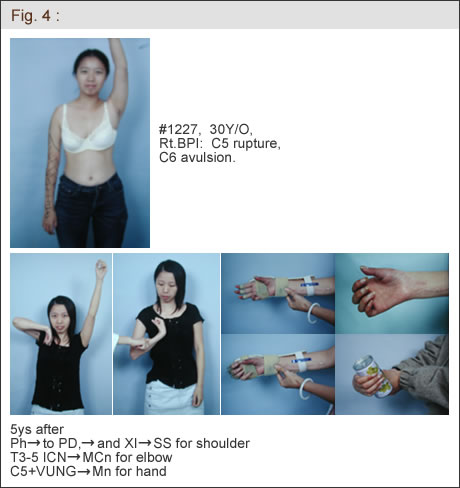
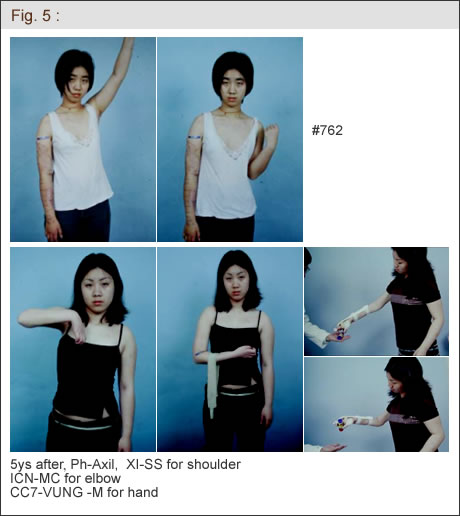
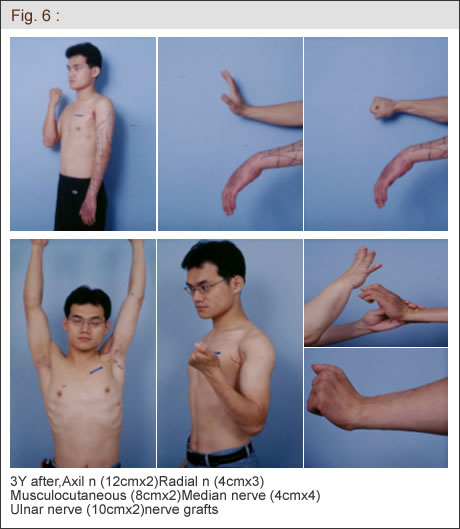
For somebody who has nothing, a little is a lot. Patients should recognize their disabilities and have to be encouraged frequently to make use of the regained but not completely recovered limb. From 1986 to 2003, 1300 adult victims of brachial plexus injury were operated in Chang Gung Memorial Hospital by the same surgeon ( D.C.C. Chuang). Cases with total root avulsions, 60˘X of shoulder elevation, M4 elbow flexion strength, M2-3 wrist and finger extension, M3 finger flexion with wrist arthrodesis were generally achieved following five years rehabilitation. ( Fig. 2-6 ). |
| |
 |
| |
 |
 |
 |
 |
|
| |
| |
|
|
|
|
|
 |

