| 銳速刀 RapidArc |
諾力刀 Novalis |
電腦刀 Cyberknife |
螺旋刀 Tomotherapy |
伽瑪刀 GammaKnife |
|
| 適應症 (治療範圍) |
全身(40 cm) | 全身(10 cm) | 全身 | 全身(較無限制) | 僅頭部(3 cm) |
| 固定效果 | 普通 | 普通~最佳 | 普通 | 普通 | 最佳 |
| 機器精確度 | 佳 | 佳 | 佳 | 佳 | 最佳 |
| 劑量分布 | 佳 | 佳 | 稍不均勻 | 佳 | 較不均勻 |
| 分次治療 | 可 | 可 | 可 | 可 | 較為困難 |
| 低劑量區域 | 普通 | 普通 | 普通 | 稍多 | 普通 |
| 治療時間 | < 5分 | <30分 | 20分~2小時 | <30分 | 20分 ~ 1小時 |
| 非同平面治療 | 可 | 可 | 一定 | 無 | 一定 |
| 影像導引 (IGRT) | 有 | 有 | 有 | 有 | 無 |
| 優點 | 快速完成360度全體積弧形放射治療減少長時間治療產生之不適 | 微細多葉準直儀 適合治療小腫瘤 |
治療中使用x光定位 可立刻修正誤差 |
治療前使用電腦斷層定位 | 固定及治療精準度高 |
| 缺點 | 計畫複雜需較久的時間做治療規畫 | 僅能治療約10公分範圍 | 許多定位照增加治療時間及低能量之輻射曝露 | 無法立刻完全修正因位移所造成之治療誤差 | 僅能做頭部的治療 放射核種隨時間衰變會增加治療時間 |
位移誤差 修正能力 |
佳 | 佳 | 佳 | 良 | |
| 價格 | 自費3萬~6萬 | 健保或自費 2~8萬 |
自費20萬或以上 (依治療次數而訂) |
自費15萬~35萬 | 健保或自費14萬 |
The Techniques of Radiotherapy
|
RapidArc |
Novalis |
Cyberknife |
Tomotherapy |
GammaKnife |
Indication (Treatment field) |
Whole Body (<40cm) |
Whole Body (<10cm) |
Whole Body |
Whole Body (no specific limit) |
Head only (<3cm) |
Fixation |
Good |
Good to very good |
Good |
Good |
excellent |
Machine accuracy |
Good |
Good |
Good |
Good |
Very good |
Dose distribution |
Good |
Good |
Slight inhomogeneity |
Good |
Slight inhomogeneity |
Fractionation |
Yes |
Yes |
Yes |
Yes |
No |
Low dose bath area |
Moderate |
Moderate |
Moderate |
More |
Moderate |
Treatment time |
<5 minutes |
<30 minutes |
20 minutes-2 hours |
<30 minutes |
20 minutes- |
Non-coplanar treatment |
Yes |
Yes |
Must |
No |
Must |
Image-Guided Radiation Therapy (IGRT) |
Yes |
Yes |
Yes |
Yes |
No |
Pros |
Rapidly deliver 360 degree volumetric Modulated Arc Therapy (VMAT) and reduce the discomfort of long treatment time. |
Use micro-multi-leaf collimator and is especially suitable for small tumor |
Use x-ray images to correct setup or positioning errors during the treatment |
Use tomography (CT) for setup localization before treatment |
High fixation and treatment accuracy |
Cons |
Due to the complexity of the plan, it takes more time for treatment planning. |
Only treat tumors smaller than 10 cm |
Repeated x-ray imaging further increases the treatment time and radiation dose |
Not able to instantly correct the treatment error caused by displacement of localization |
Only can treat small head leions. Treatment time will be increased as radioactive sources decay. |
Capability for Setup error correction |
Good |
Good |
Good |
Fair |
Not applicable |
Price |
Self-pay 30,000-60,000 NTD |
National Insurance or Self-pay 20,000-80,000 NTD |
Self-pay above 200,000 NTD (depends on number of treatments) |
Self-pay 150,000-350,000 NTD |
National Insurance or Self-pay 140,000 NTD |
Comparison of treatment techniques
放射治療(俗稱電療)的進步,在這幾年由報章雜誌的報導頻率,便可見一般。治療的機器,過去刻板印象中的鈷60,早已被直線加速器所取代。直線加速器可提供較高能量的放射線,可穿透較深的組織,且對體表的傷害較低。然而隨著科技的進展,機器的精細及治療計畫的複雜程度,皆非10年前所能比擬。廠商們也根據不同原理,設計出各有特色的治療機器,希望能提供患者最好的治療效果。
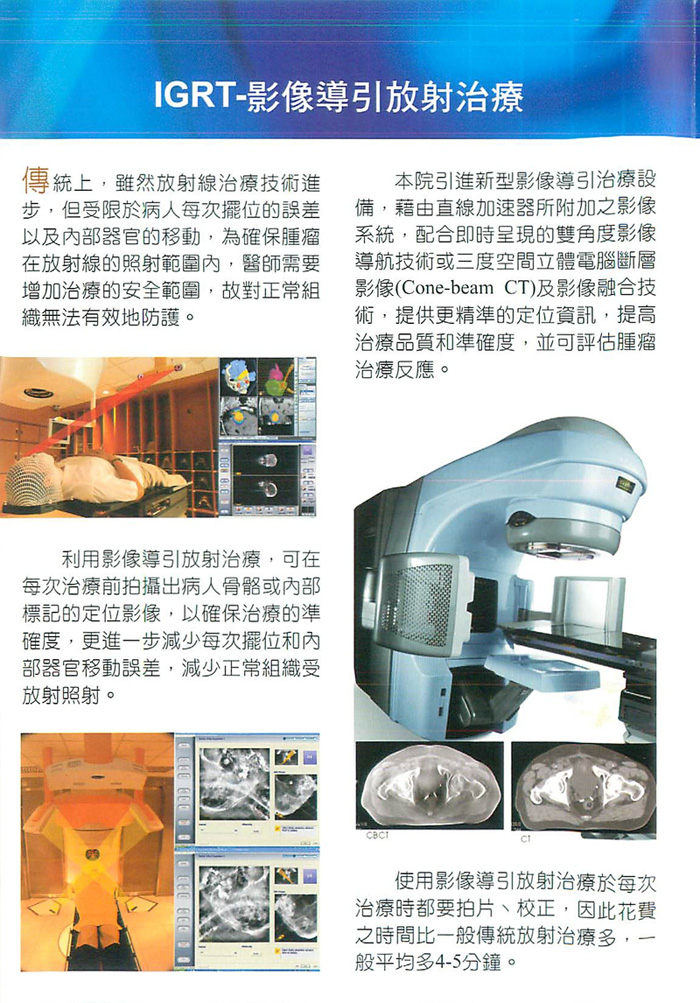
經過加裝相關設備,傳統的直線加速器也可施行大多數的特殊的放射治療。例如在射束出口加上多葉準直儀,及有合適的治療計畫系統,便能進行強度調控(IMRT)的治療。所謂強度調控,意指在同一照野下,有不同的放射線強度。這種治療方式,對於深度不一或是形狀不規則的腫瘤,有較好的包覆性,且對正常組織傷害較小,腫瘤內的劑量分布也較為均勻。而影像導引放射治療,可藉由再次的影像確定治療位置及範圍,減少治療的誤差。
然而傳統機器較不適用於單次高劑量的治療,例如放射手術。長時間的治療,若無很好的固定方法,會引起相當大的誤差,所以伽瑪刀便利用腦部手術定位的頭架固定方式,來達到最佳的固定效果。伽瑪刀使用二百多顆固定角度的鈷60射源,其射束集中至一點,治療時將病灶移到劑量集中點,便可在短時間給予相當高的劑量。而好的病患固定系統加上固定角度的射源,給予伽瑪刀在各種腦部放射治療機器中,最小的治療誤差。但是其高劑量區成一圓球形,若腫瘤形狀為不規則形,便需要利用多個中心點的圓球劑量分布來組成治療所需形狀,這種治療方式導致伽瑪刀常是劑量分布最不均勻的治療方式。另一方面,伽瑪刀因其設計為頭盔式的射源,故僅能運用於腦部或頭部治療,而射束大小也限制其適合病灶約在3公分左右。運用跟伽瑪刀相似的原則,傳統的直線加速器若加上相關配備也可施行放射手術治療,其劑量分布甚至優於伽瑪刀,但是因機器上的限制,其準確度稍差,但多還在2mm之內。
為進一步改善傳統直線加速器治療機用於放射手術的缺點,諾力刀使用較精細的機器使誤差降低到1mm左右,高劑量輸出來減少治療時間,而微細多葉準直儀使利用單一中心點治療不規則形狀的腫瘤成為可能,進而有很好的劑量分布,而非頭架的固定方式可運用於多次治療,以減少高劑量單一次照射所可能引發的副作用。若運用於顱外的治療,諾力刀可運用互成直角的兩個X光射源做影像導引的放射治療(IGRT),來校正治療的位置。然而其影像導引僅用於治療前的定位,但並無法即時修正位置,故在諾力刀的治療中,選擇好的固定系統仍然相當重要。
目前僅有電腦刀可在治療中監測病患位置。電腦刀同樣利用兩個X光射源做影像導引的根據,在治療中會再擷取影像作為定位的修正參考,每次治療可能會照數十到上百張X光,稍增加低劑量的輻射曝露,也會因多次再對位而使治療時間延長。電腦刀利用機器手臂控制小型直線加速器的位置,在空間中運用類似伽瑪刀的圓錐狀射束,可從上百個不同角度來做治療。因其可選擇角度眾多,對正常組織有不錯的閃避能力,但是其射束形狀及強度固定,所以劑量均勻性稍差。
而螺旋刀是運用電腦斷層的概念,將高能的放射線束用來治療及造影。螺旋刀的治療是將射束如同螺旋般繞病患治療,利用快速多葉準直儀控制劑量的給予,這種繞轉的治療方式,可在同平面上產生相當好的高劑量分布曲線,但是同時也有較廣泛的低劑量區域,而且並沒辦法進行非同平面的治療。在影像導引方面,不同於諾力刀及電腦刀利用骨骼來定位,螺旋刀可在每次取像中直接看見腫瘤所在位置,以減少治療誤差。但因其治療計畫需時甚久,現仍無法根據斷層所顯示腫瘤變化更改治療參數,且因其機械結構關係,並不能像諾力刀或電腦刀輕易修正病患位置。
整體而言,現今的放射治療技術已較過去有長足的進步,一般的治療機器誤差多在5mm以內,而上述介紹的機器誤差皆在2mm以內,能夠符合高精確程度治療的需求。但是腫瘤治療並不是僅有好的機器便可,一個好的治療團隊,包括內外科、診斷科、放射治療科,及物理師平時對這些機器的保養及品質管控,才能確保治療的品質,否則號稱最準確的伽瑪刀治療後發現位置有明顯誤差,也偶有所聞。選擇治療機器前,尤其是高劑量少次數精密治療,多聽多看才能確保自身的權益。
Since Cobalt-60 unit was well known as a machine for radiotherapy, same concept was remained in general population. However, linac accelerator provides x-ray with engery higher than gamma ray from Cobalt-60 unitand this higher energy x-ray penetrates into deeper tissues and protects dmages in the superficial tissues. With the advance of technology, a varity of machines with unique characteristics were designed by different vendors to fit the needs of clinical application..
Conventional linac accelerator (Linacs) can perform most of the routine radiation therapy techniques.. For example, with add-on Multi-leaf collimator (MLC) and appropriate treatment planning system (TPS), most of the Linacs can deliver Intensity Modulated Radiation Therapy (IMRT) IMRT means we are able to have different radiation intensity at different regions insdie the one treatment field. IMRT technique has the adventage of beter conformity for irregular tumor shape as compared to conventional three-dimensional radiation therapy (3D CRT). The dose distribution inside the tumor is also more uniform However, the conventional linac accelerator is not suitable for high-dose single fraction treatment such as radiosurgery (SRS) for brain tumor, due to its larger MLC width and limited angles for non-coplaner treatment .A good fixation system is also required to reducethe setup error in SRS. Thus, gamma knife utilizes the head frame used for brain surgery as a fixation tool to achieve the best fixation. Gamma knife uses over 200 Cobalt-60 sources from fixed but different angles to focus on the same spot, and tumor is moved tothis focus spot to receive fairly high dose radiation in a short period of time. The fixation system and fixed-angle sources design in Gamma knife provides best fixation and least setup errors among all types of equipment for SRS of brain. However, the high-dose area forms in round shape and multiple centers are required for an irregular tumor. Thoverlap of doses from multiple centers causes the most inhomogenous dose distribution as compared to other techniques. The distribution of radioactive sources is in helmet shape in Gamma Knife, which made it can be only used on brain or head treatment. The size of the radiation source limits the size of suitable tumor to around 3cm as well. SRS can be performed by conventional Linacs with ancillary devices and the dose distribution is comparable to Gamma Knife; but the accuracy of whole system is within 2mm which is slightly inferior to Gamma Knife. In order to improve the machine accuracy, Novalis uses more sophiscated devices to improve the accuracy to be less than 1mm. Novalis has high dose rate to decrease the treatment time, micro multileaf collimator to shape irregular tumor with one single focus center , and frameless fixation for fractionated treatment to minimize the possible side effect from a single, high dose treatment. For extra-cranial treatment, Novalis provided two orthogonal x-ray images as pre-treatment image-guided radiation therapy (IGRT) verification. However, this IGRT technique can be only used before treatment, and not able to correct setup error instantly during the radiotherapy. Therefore, the choice of fixation device on Novalis machine still plays an important role.
Currently, only cyberknife can detect the setup error of the patients during the treatment. Cyberknife also use two x-ray images as IGRT reference, and performs repeated x-ray images as setup localization. It may take ten to hundreds x-ray images in every treatment; this increases radiation exposure and also increases the treatment time. Cyberknife utilizes robotic arm to control the location of the mini Linacs; it can perform the treatment from hundreds of angles, thus it provides relatively good normal organ sparing. However, its beam shape and intensity is fixed and the dose homogeneity is relatively worse due to the overlapping of fixed beam shape..
Tomotherapy borrows the concept of tomography (CT) in diagnostic radiology, and uses high-energy radiation beam for treatment and imaging. Tomotherapy perform the radiation therapy in spiral direction around the patient and use fast multileaf collimator to control the given dose. This kind of spiral treatment can have very good dose distribution in coplanar direction, but it has more low dose region and is not able to perform non-coplanar treatment. In the aspect of IGRT, Tomotherapy can visualize the location of tumors after IGRT and minimize treatment error. However, the treatment planning time is long, Tomotherapy can’t change treatment parameters according to changes of tumor . Due to its mechanical limitation, it can’t easily correct patient position like Novalis or Cyberknife.
In general, the radiation therapy technique evolved rapidly and most of the machines have the error less than 5mm and the machine we described above could achieve error within 2mm and fit the need of high precision treatment. However, asuccessful cancer treatment not only lies on a good machine, but more importantly needs a strong team including surgeon, medical oncologist, radiation oncologist, radiologist and many specialitist, The medical physicist plays important role in performing the quality assurance of whole treatment system, and assuring the treatment quality. Before making a choice on treatment machine and technique, we recommend you to search and learn more information, so that the possibility for you to have the most appropriate treatment will be maximized..
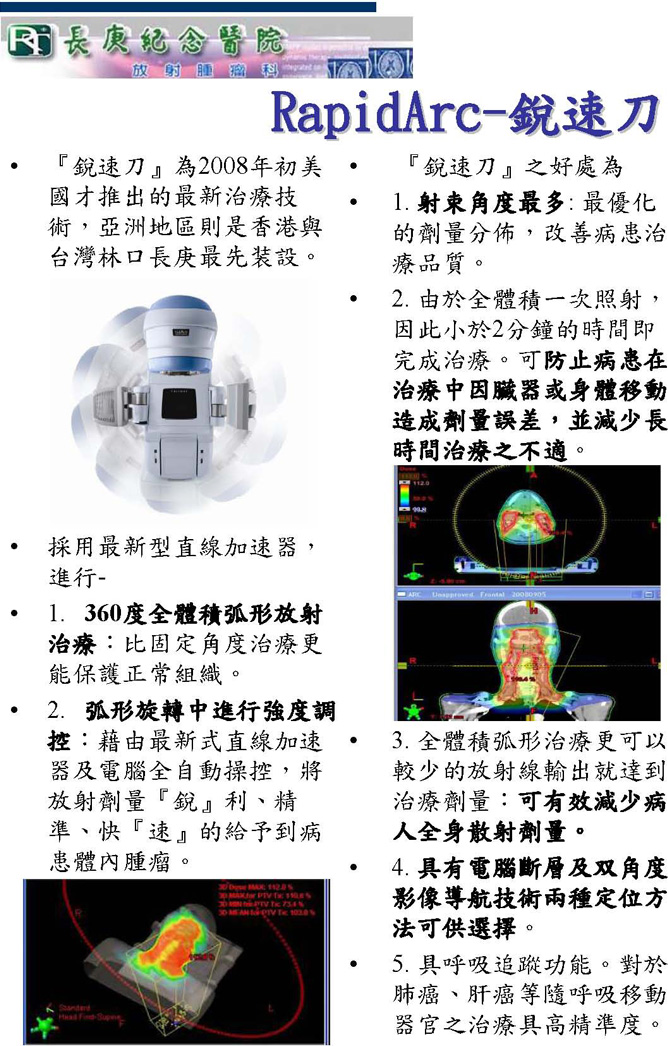
RapidArc® is an advanced technology from Varian Medical Systems that improves dose conformity to the tumors while significantly shortens treatment time. The first installation in Asia took places in Taiwan and Hong Kong, and CGMH was the first hospital in Taiwan to install this newest technique.
- RapidArc is a volumetric arc therapy that delivers a precisely sculpted 3D dose distribution with a single 360-degree rotation of the linear accelerator gantry.
- Volumetric modulated arc therapy differs from existing techniques like helical IMRT or intensity-modulated arc therapy (IMAT), because it delivers dose to the whole volume, rather than slice by slice. The treatment planning algorithm ensures the treatment precision and spares normal healthy tissue.
Advantages
- A single arc can deliver essentially similar dose distributions compared with IMRT plans that incorporate as many as 36 fields, in other words, RapidArc can improve treatment quality because it has more angle to modulate the dose distribution.
- RapidArc delivers treatments two to eight times faster than our fastest dynamic treatments today and increases precision. It takes less than two minutes to finish one treatment – can reduce dose error caused by tumors that move during treatment as the patient breathes in and out.
- As compared with IMRT, volumetric arc therapy can use less radiation output to match with the same prescribed dose. It can reduce scattered dose to the patient.
It has Cone Beam Computed Tomography (CBCT) and On-Board Imager (OBI) image-guided technologies.
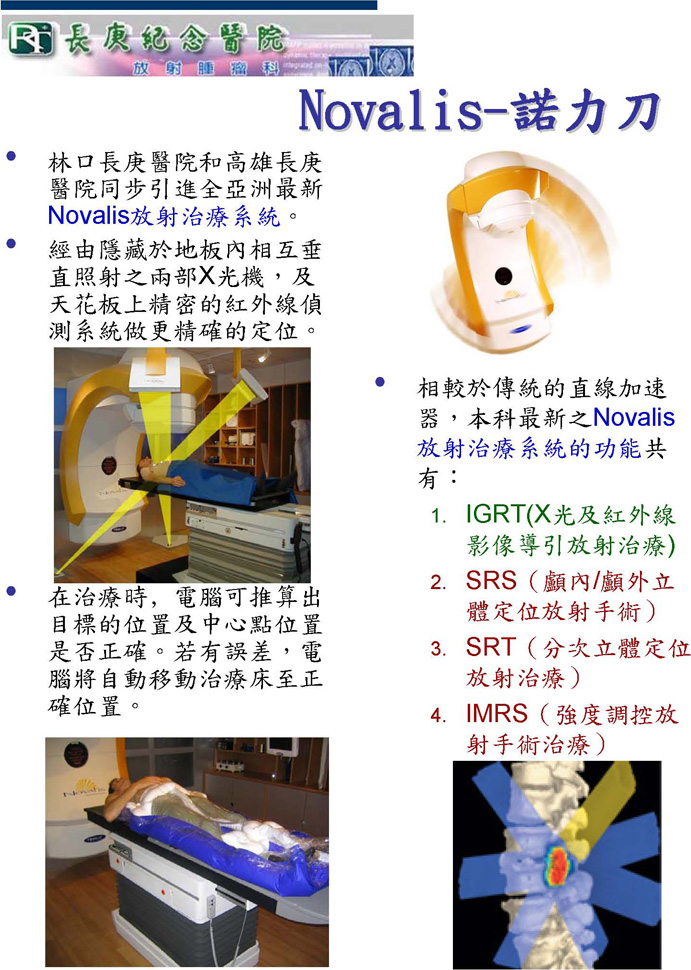
As compared with other modalities for radiosurgery, Novalis provides the better treatments at equivalent or even better accuracy, faster treatment delivery, more flexible treatment scheduling and higher level of patient comfort.
ROOM BASED X-RAY IMAGING
- ExacTrac has two x-ray tubes on the floor which are perpendicular to each other. It performs localization correction in two minutes.
- X-ray IGRT images are verified automatically and patient setup, including corrections with 6 degree freedom, is accurately adjusted for streamlined workflow and throughput.
- Compared with traditional linac, the Novalis Radiosurgery System can perform:
- Imaged Guided Radiotherapy (IGRT) – inclusive of x-ray and infrared imaged guided radiotherapy.
- Stereotactic Radiosurgery (SRS) – cranial and extra-cranial stereotactic radiosurgery.
- Stereotactic Radiotherapy (SRT) – fractionated stereotactic radiotherapy.
- Intensity-Modulated Radiosurgery (IMRS)
Stereotactic radiotherapy (SRS) – SRS is a targeting radiotherapy which is aimed at the tumor from many different angles. Using this method, it can effectively destroy small malignant tumors, suppress the growth of benign lesions, or close down abnormal blood vessels.
This technique, which is accurate to sub-millimeter level, does not require surgery and can be done on an outpatient basis.
Stereotactic radiosurgery includes the participation of both the surgical and radiation oncology members who work together to treat every patient.
The radiotherapy beam is accurately targeted during the SRS. It is vitally important that patient’s head is in exactly the same position each time and does not move while they are being treated.
IGRT technology ensures the radiotherapy is targeted to the same position during every treatment session. IGRT provides high-resolution, three-dimensional images to pinpoint tumor or reference site. Patient’s position is adjusted accordingly when necessary.
Through more precise targeting of the beam to tumors, doses to the tumors might be increased and to the non-target volumes can be reduced. Higher radiation doses have been shown to enhance tumor control and better sparing on non-target regions reduces the possibility of side effects after radiotherapy.
On-Board Imager® kV imaging system with cone-beam CT
- Fully automated real-time imaging system enables clinicians to pinpoint tumor sites, adjust positioning, and complete a treatment all within the standard timeslot
- On-Board Imager operates along three axes of motion for optimum positioning
- High precision image tracker shows internal anatomic landmarks and tracks motion
- Toolkit includes radiographic 2D imaging, and fluoroscopic and 3D cone-beam CT for fine tuning patient positioning just prior to treatment
- Volumetric cone-beam CT provides a high-quality 3D image to help distinguish tumors from surrounding soft tissue and improve tumor targeting
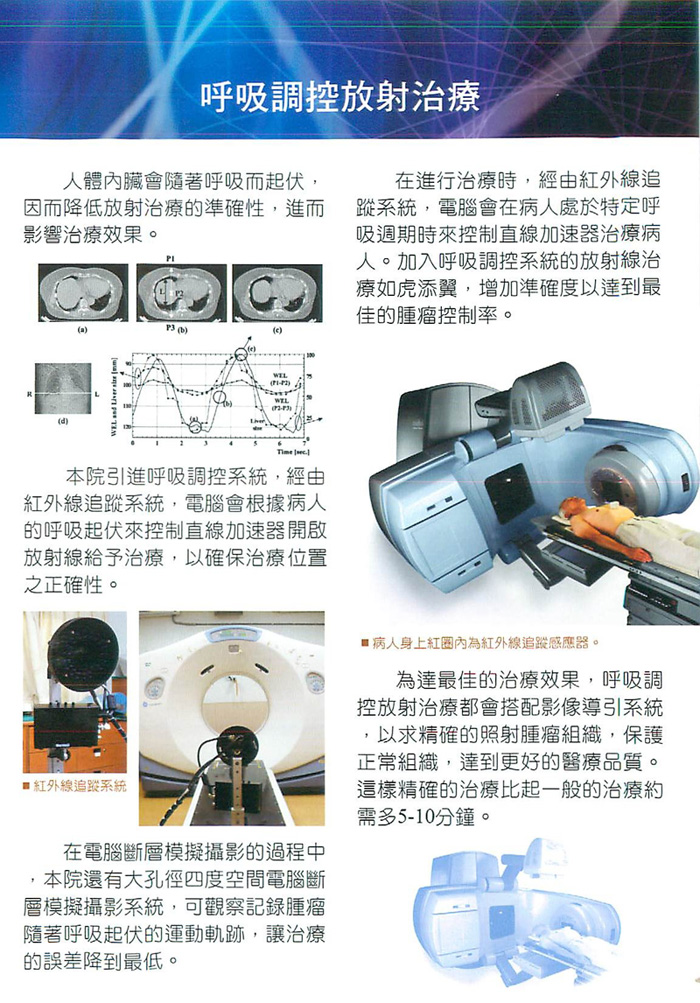
Respiratory gating technique which tracks tumors that move during treatment as the patient breathes in and out, such as lung and liver cancer, and treats it within the gated phase with high accuracy.
CGMH introduces Real-time Position Management (RPM) respiratory gating system which gates the beam delivery during treatment to account for organ motion. Treatment parameters are adapted in real time to conform to the patient anatomy. This system combines continuous monitor chest wall movement during treatment with pre-plotted target trajectories to ensure the maximum dose is delivered to the target while avoiding critical organs. In this case, we can treat patients with high accuracy while minimize treatment errors.
- Real-time Position Management™ (RPM) system
Non-invasive automated system synchronizes breathing motion with image acquisition. Radiation beam is gated to when the target falls within the treatment field. Patient can breathe normally and remain comfortable and high compliance.
放射治療與手術的結合
Intra-Operative Radiotheraphy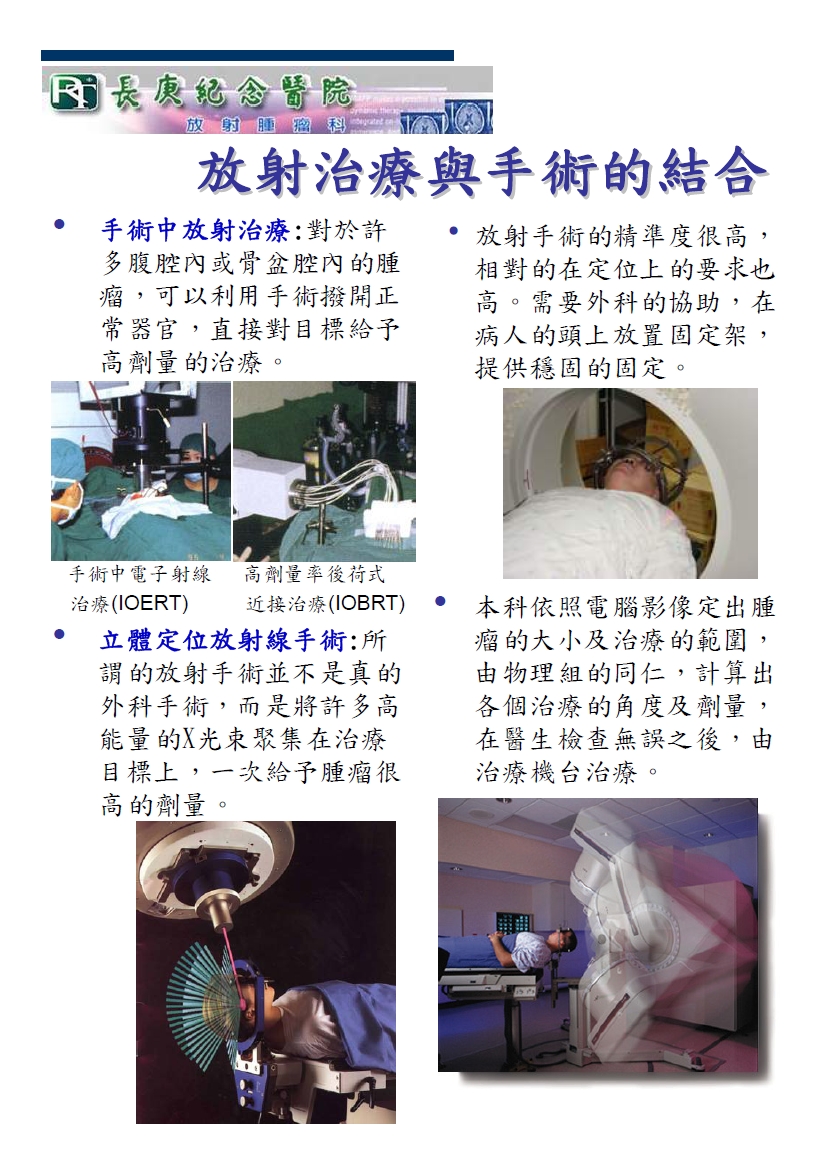 Intraoperative Therapy – Intraoperative radiation therapy (IORT) delivers a single, high dose of radiation therapy to a tumor bed during surgery. This advanced technology may help eradicate residual tumor cells, reduce radiation treatment time or provide an added radiation "boost" to external beam radiotherapy. The rationale for IORT is to deliver a high dose of radiation precisely to the targeted area with minimal exposure of surrounding tissues which are displaced or shielded during the IORT. IORT can both be performed with electron beams (IOERT) and gamma-rays.
Intraoperative Therapy – Intraoperative radiation therapy (IORT) delivers a single, high dose of radiation therapy to a tumor bed during surgery. This advanced technology may help eradicate residual tumor cells, reduce radiation treatment time or provide an added radiation "boost" to external beam radiotherapy. The rationale for IORT is to deliver a high dose of radiation precisely to the targeted area with minimal exposure of surrounding tissues which are displaced or shielded during the IORT. IORT can both be performed with electron beams (IOERT) and gamma-rays.
呼吸調控放射治療
Respiratory gating Radiotheraphy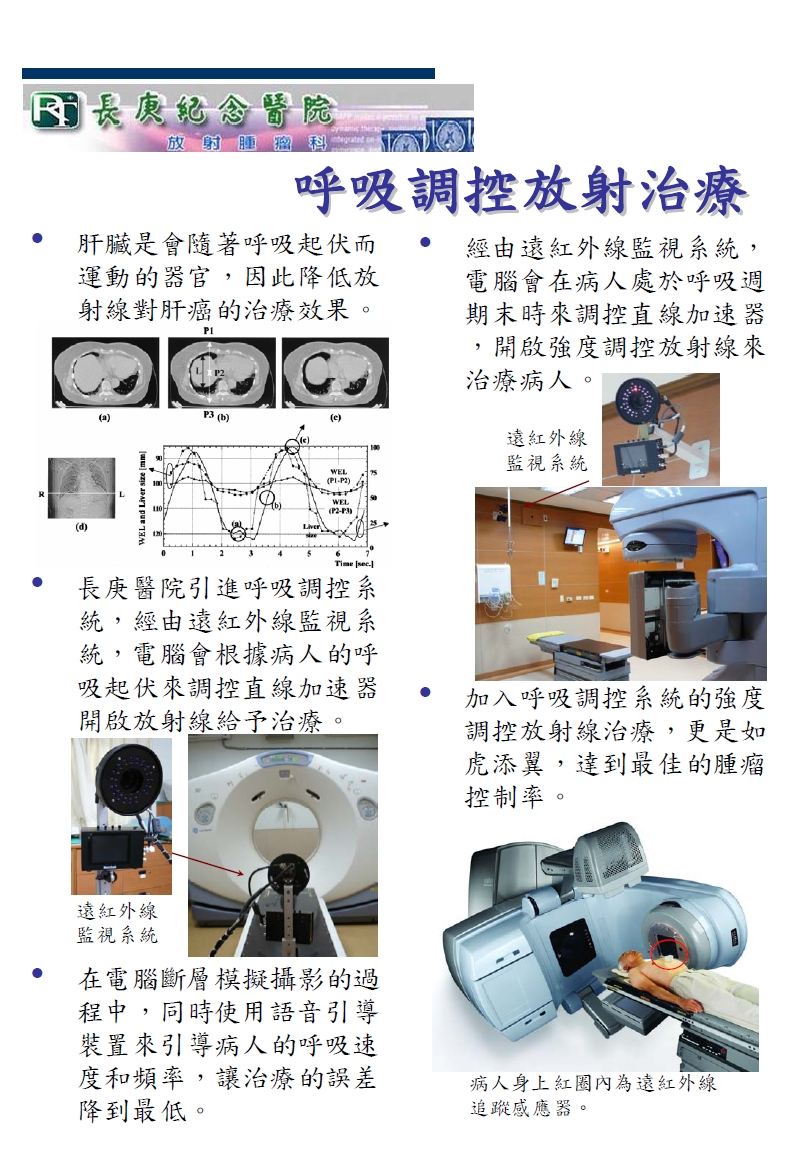
Respiratory gating technique which tracks tumors that move during treatment as the patient breathes in and out, such as lung and liver cancer, and treats it within the gated phase with high accuracy.
CGMH introduces Real-time Position Management (RPM) respiratory gating system which gates the beam delivery during treatment to account for organ motion. Treatment parameters are adapted in real time to conform to the patient anatomy. This system combines continuous monitor chest wall movement during treatment with pre-plotted target trajectories to ensure the maximum dose is delivered to the target while avoiding critical organs. In this case, we can treat patients with high accuracy while minimize treatment errors.
- Real-time Position Management™ (RPM) system
Non-invasive automated system synchronizes breathing motion with image acquisition. Radiation beam is gated to when the target falls within the treatment field. Patient can breathe normally and remain comfortable and high compliance.
強度調控放射治療
Intensity-Modulated Radiation Therapy (IMRT)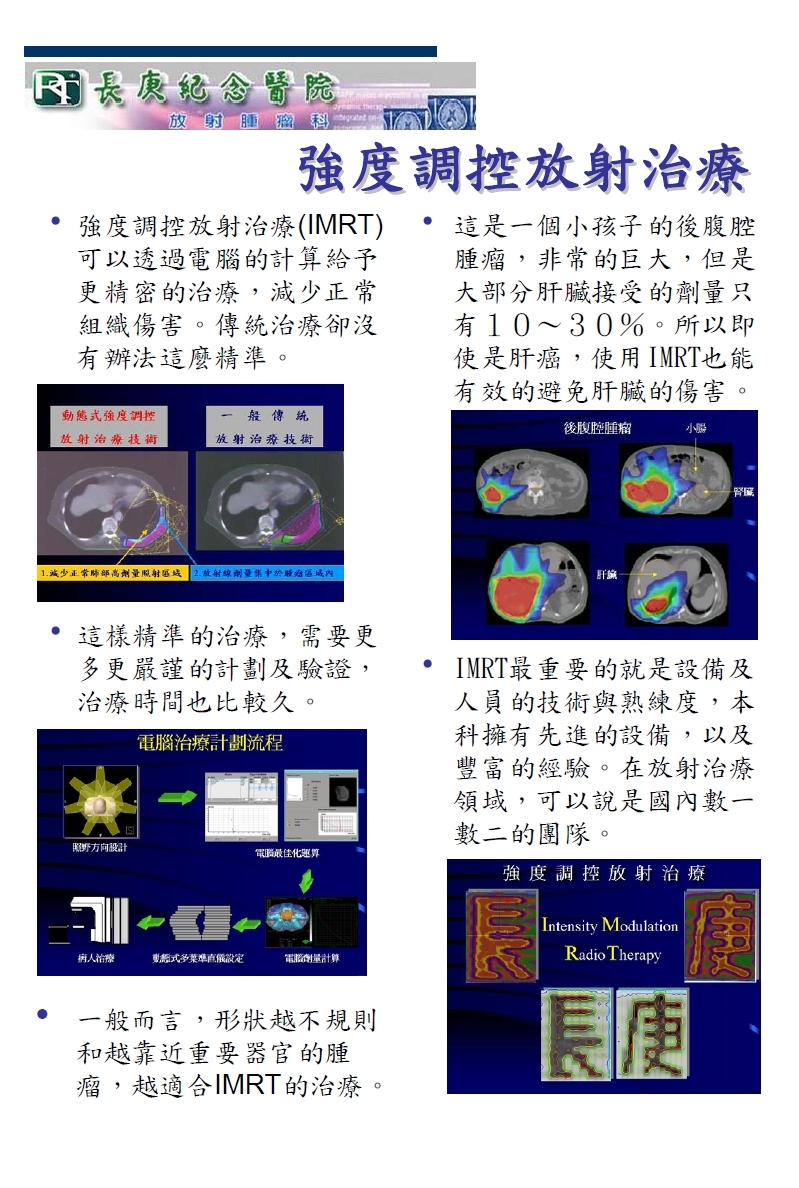
-
Intensity-Modulated Radiation Therapy (IMRT) performs precise treatment through inverse planning calculation. Higher radiation doses can be delivered directly to tumors, while surrounding organs and tissues are protected. This advantage in dose distribution can’t be achieved by traditional radiation therapy.
-
As compared with traditional treatment plan, IMRT plan needs more time to do the optimization and dose calculation because of its complexity and the requirement of high precision.
-
In general, IMRT technique is more suitable for tumors with irregular shapes or close to the critical organ. Lower doses to critical normal tissues may translate into less complications or side effects. For example, in the case of head and neck tumors, IMRT minimizes radiation exposure of the spinal cord, optic nerve, salivary glands or other critical structures.
-
Most importantly, the execution of a successful IMRT treatment requires good equipment and a strong, experienced team including physicians, physicists, and therapists. Our team can provide you the best service.
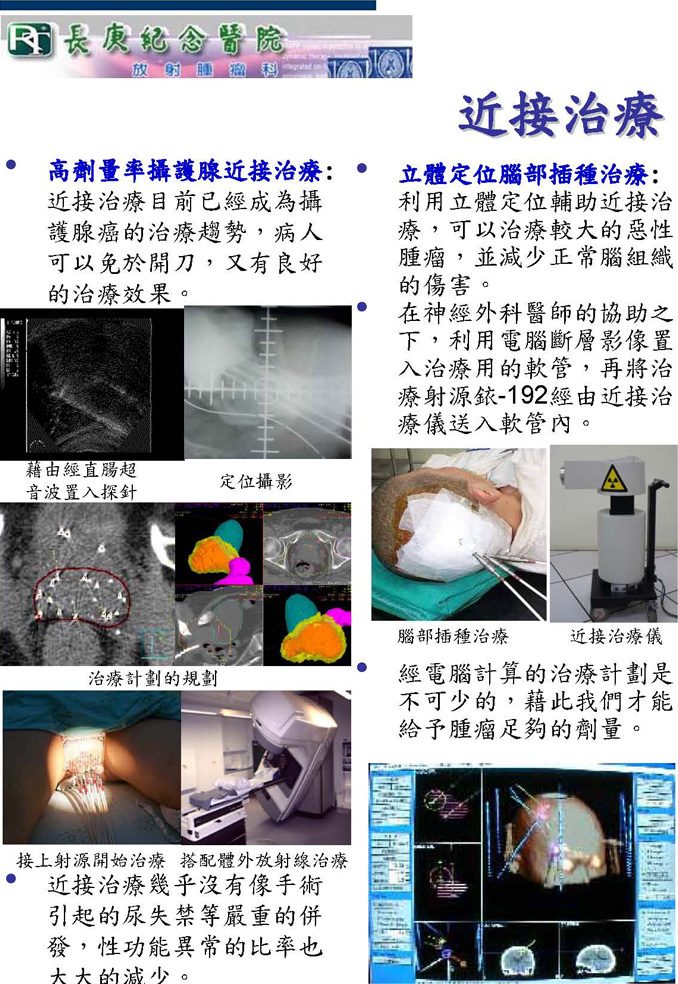
Brachytherapy is to place radioactive sources directly into or next to the tumor or target region. This enables tumors to be treated by high radiation dose but a rapid dose fall-off to the surrounding healthy tissues.
High-Dose-Rate (HDR) brachytherapy uses a higher-strength radioactive source contained within an afterloader device. The afterloader delivers the source for a short period of time to catheters, needles, or other appliances placed in the tumor site.
- HDR prostate cancer brachytherapy—Brachytherapy has become the treatment trend for early stage prostate cancer. Patients don’t need surgery but yet have good treatment outcome. Patients treated by HDR brachytherapy have much lower incidence of urinary incontinence as compared with radical surgery, furthermore, the probability of sexual dysfunction is also significantly reduced.
- Stereotactic Brain Implant—The use of stereotactic localization to assist brachytherapy can treat larger brain tumor but reduce normal brain complication. By cooperation with neurosurgeon, computed tomography is used to check the right position of applicator, and Ir-192 source entered into the target site through afterloader device.
- Three dimension computer treatment planning to perform dose calculation and ensure tumor coverage is essential for brachytherapy.
未來發展-質子治療
In the Future-Proton Theraphy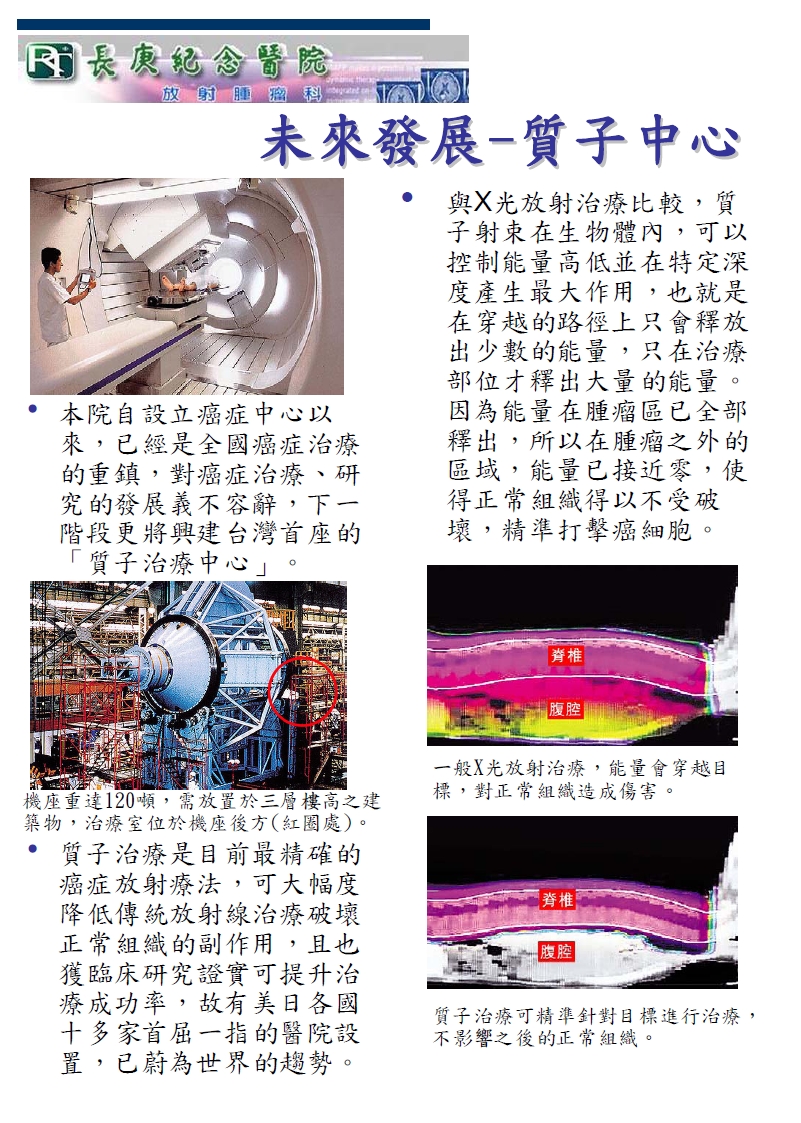
-
The Proton Advantage
The energy of proton beam is selected so that the Bragg peak coincides with the treatment depth. Since nearly all the tumors in the clinics are larger than the width of one Bragg peak, a Spread-Out Bragg Peak (SOBP) by superimposing multiple beams with different energies is required. The Bragg peak or SOBP ensures a limited dose deposition in the entrance region and no exit dose behind the target volume. This greatly improves dose conformity and the ability to spare healthy tissue and allows clinicians to treat tumors close to vital organs.
