|
|
|
|
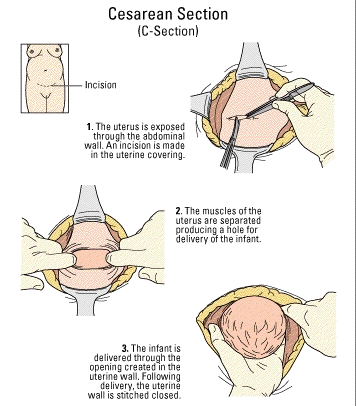
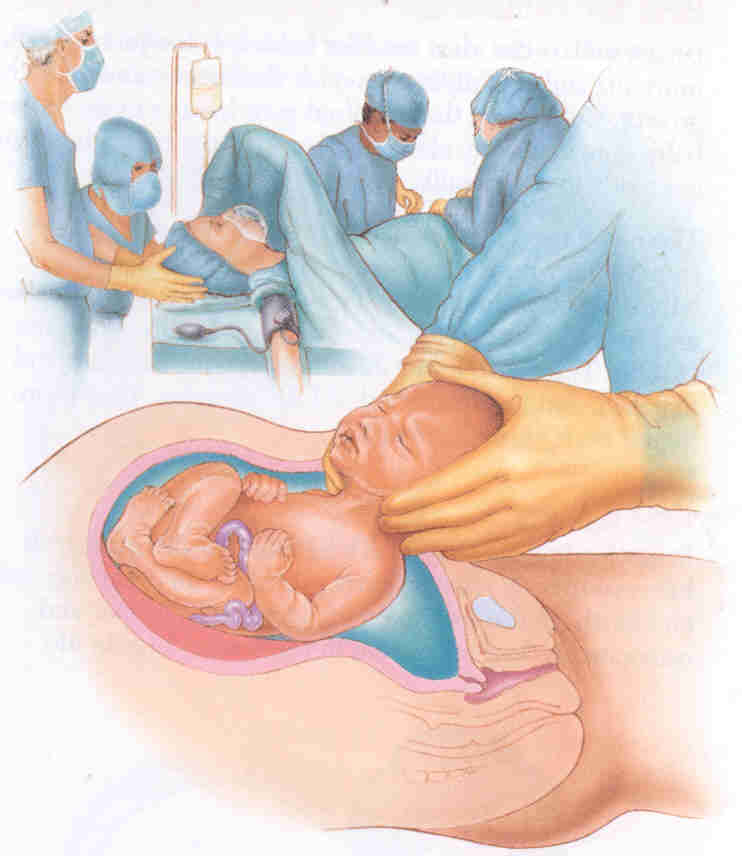
A C-section delivery is performed when a vaginal birth is not possible or is not safe for the mother or child. Surgery is usually done while the woman is awake but pain-free from the chest to the legs (epidural or spinal anesthesia). An incision is made across the abdomen just above the pubic area. The uterus is opened, the amniotic fluid is drained off, and the baby is delivered. The baby's mouth and nose are cleaned of fluids and the umbilical cord is clamped and cut. The baby is handed to the pediatrician or nurse who will make sure that he is breathing well. The mother is awake and she can hear and see her baby. Due to increased medicalization of birth, C-sections have become fairly common (up to 20% of all births in the U.S.). |
| |||||||||||||||||||||||
 |
 |
ˇ@ | ||||||||||||||||||||||
|
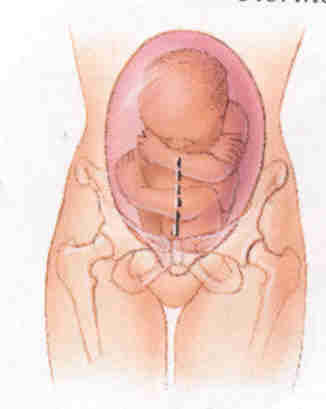
Vertical Inscision |
Horizontal or Bikini Inscision |
| ||||||||||||||||||||||
Indications
Some of the main reasons for C-section delivery instead of vaginal delivery include the following
|
|
decreased oxygen level |
|
multiple babies in the uterus (multiple births) |
|
|
increased or decreased heart rate |
|
problems with the cervix |
|
|
problems with the uterus |
|
too loose or relaxed (incompetent cervix) |
|
|
too small, scarred, or deformed |
|
active genital herpes infection of the mother |
|
|
problems with the placenta and umbilical cord |
|
abnormally developed baby |
|
|
attached too close to the cervix (placenta previa) |
|
"buttocks-first" delivery (breech presentation) |
|
|
baby's head is too large to pass through mother's pelvis (cephalopelvic disproportion) |
|
crosswise (transverse) position |
|
|
prolonged labor |
|
pregnancy at older age (over 40 years |
|
|
abnormal position of the baby |
|
extreme illness (toxemia, preeclampsia, eclampsia, hypertension) |
|
|
incompletely attached to the uterus (placenta abruptio) |
Convalescence:
|
The average hospital stay is 2 to 4 days. Recovery takes longer than it would from a natural birth. Walking is encouraged the day of surgery to speed recovery. Pain can be managed with oral medications. |
Risks
|
|
reactions to medications |
|
infection of the bladder or uterus |
|
|
problems breathing |
|
infection of the uterus |
|
|
bleeding |
|
back pain |
| ˇ@ | ˇ@ | ˇ@ | ˇ@ |
|
PROBLEMS DURING SURGERY • If the uterus is atonic, continue to infuse oxytocin and give ergometrine 0.2 mg IM and prostaglandins, if available. These drugs can be given together or sequentially (Table S-8). • Transfuse as necessary. • Have an assistant press fingers over the aorta to reduce the bleeding until the source of bleeding can be found and stopped. • If bleeding is not controlled, perform uterine and utero-ovarian artery ligation or hysterectomy.
• Complete the delivery as in a vaginal breech delivery:
BABY IS TRANSVERSE • Grasp the ankles and pull gently through the incision to deliver the legs and complete the delivery as for a breech baby. THE
BABYˇ¦S BACK IS DOWN • After the incision is made, reach into the uterus and find the feet. Pull them through the incision and complete the delivery as for a breech baby. • To repair the vertical
incision, you will need several layers of suture. PLACENTA PRAEVIA • After delivery of the baby, if the placenta cannot be detached manually, the diagnosis is placenta accreta, a common finding at the site of a previous caesarean scar. Perform a hysterectomy. • Women with placenta praevia are at high risk of postpartum haemorrhage. If there is bleeding at the placental site, under-run the bleeding sites with chromic catgut (or polyglycolic) sutures. • Watch for bleeding in the
immediate postpartum period and take appropriate action. POST-PROCEDURE CARE • If bleeding occurs:
• If there are signs of infection or the woman currently has fever, give a combination of antibiotics until she is fever-free for 48 hours:
• Give appropriate analgesic drugs.
• Use a scalpel to make the incision:
• Ask an assistant (wearing high-level disinfected gloves) to apply pressure on the cut edges to control the bleeding. • Cut down to the level of the membranes and then extend the incision using scissors. • After rupturing the membranes, grasp the babyˇ¦s foot and deliver the baby. • Deliver the placenta and membranes. • Grasp the edges of the incision with Allis or Green Armytage forceps. • Close the incision using at least three layers of suture:
• Close the abdomen as for lower segment caesarean section (page P-48). The woman should not labour with future pregnancies.
• Review for consent of patient. • Grasp the least vascular, middle portion of the fallopian tube with a Babcock or Allis forceps. • Hold up a loop of tube 2.5 cm in length (Fig P-24 A). • Crush the base of the loop with artery forceps and ligate it with 0 plain catgut suture (Fig P-24 B). • Excise the loop (a segment 1 cm in length) through the crushed area (Fig P-24). • Repeat the procedure on the other side. ˇ@ |
|||
ˇ@