|
Normal
labour and childbirth
NORMAL LABOUR
• Make a rapid evaluation of the general
condition of the woman including vital signs
(pulse, blood pressure, respiration,
temperature).
• Assess fetal condition:
- Listen to the fetal heart rate immediately
after a contraction:
- Count the fetal heart rate for a full
minute at least once every 30 minutes during
the active phase and every 5 minutes during
the second stage;
-
If there are fetal heart rate
abnormalities (less than 100 or more
than 180 beats per minute), suspect fetal
distress.
-
If the membranes have ruptured, note
the colour of the draining amniotic fluid:
-
Presence of thick meconium indicates the
need for close monitoring and possible
intervention for management of fetal
distress
-
Absence of fluid draining after rupture of
the membranes is an indication of reduced
volume of amniotic fluid, which may be
associated with fetal distress.
SUPPORTIVE CARE DURING LABOUR AND CHILDBIRTH
•
Encourage the woman to have personal support
from a person of her choice throughout labour
and birth:
-
Encourage support from the chosen birth
companion;
-
Arrange seating for the companion next to
the woman;
-
Encourage the companion to give adequate
support to the woman during labour and
childbirth (rub her back, wipe her brow with
wet cloth, assist her to move about).
•
Ensure good communication and support by
staff:
-
Explain all procedures, seek permission and
discuss findings with the woman;
-
Provide a supportive, encouraging atmosphere
for birth, respectful of the woman��s wishes;
-
Ensure privacy and confidentiality.
•
Maintain cleanliness of the woman and her
environment:
-
Encourage the woman to wash herself or bathe
or shower at the onset of labour;
-
Wash the vulval and perineal areas before
each examination;
-
Wash your hands with soap before and after
each examination;
-
Ensure cleanliness of labouring and birthing
area(s);
-
Clean up all spills immediately.
•
Ensure mobility:
-
Encourage the woman to move about freely;
- Support the
woman��s choice of position for birth.
•
Encourage the woman to empty her bladder
regularly.
Note:
Do not routinely give an enema to women in
labour.
•
Encourage the woman to eat and drink as she
wishes. If the woman has visible severe
wasting or tires during labour, make sure
she is fed. Nutritious liquid drinks are
important, even in late labour.
•
Teach breathing techniques for labour and
delivery. Encourage the woman to breathe out
more slowly than usual and relax with each
expiration.
•
Help the woman in labour who is anxious,
fearful or in pain:
-
Give her praise, encouragement and
reassurance;
-
Give her information on the process and
progress of her labour;
-
Listen to the woman and be sensitive to her
feelings.
•
If the woman is distressed by pain:
-
Suggest changes of position (Fig
C-2);
-
Encourage mobility;
-
Encourage her companion to massage her back
or hold her hand and sponge her face between
contractions;
-
Encourage breathing techniques;
-
Encourage warm bath or shower;
-
If necessary, give pethidine 1 mg/kg body
weight (but not more than 100 mg) IM or IV
slowly or give morphine 0.1 mg/kg body
weight IM.
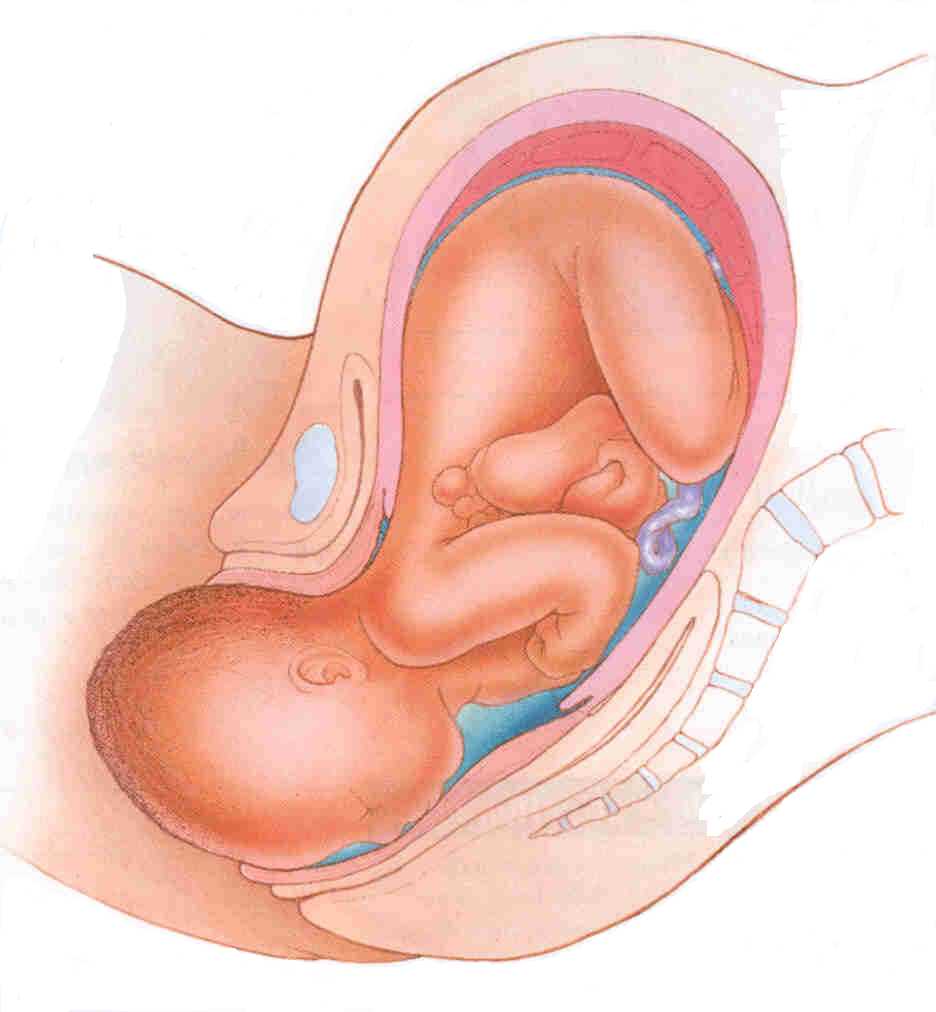
Figure
C-2
Positions that a woman adopt during labour
DIAGNOSIS
Diagnosis of labour includes:
• diagnosis and confirmation of labour;
• diagnosis of stage and phase of labour;
• assessment of engagement and descent of the
fetus;
• identification of presentation and position
of the fetus.
An incorrect diagnosis of labour can lead to
unnecessary anxiety and interventions
�@
DIAGNOSIS AND CONFIRMATION OF LABOUR
•Suspect or anticipate labour if the woman
has:
- intermittent abdominal pain after 22 weeks
gestation;
- pain often associated with blood-stained
mucus discharge (show);
- watery vaginal discharge or a sudden gush
of water.
•Confirm the onset of labour if there is:
- cervical effacement�Xthe progressive
shortening and thinning of the cervix during
labour; and
- cervical dilatation�Xthe increase in
diameter of the cervical opening measured in
centimetres (Fig
C-3 A�VE).
Figure C-3
Effacement and dilatation of the cervix
Table C-8 Diagnosis of stage and phase of
labour a
|
Symptoms and Signs |
Stage |
Phase |
|
• Cervix not dilated |
False labour/
Not in labour |
|
|
• Cervix dilated less than 4 cm |
First |
Latent |
|
• Cervix dilated 4�V9 cm
• Rate of dilatation typically 1 cm per
hour or more
• Fetal descent begins |
First |
Active |
|
• Cervix fully dilated (10 cm)
• Fetal descent continues
• No urge to push |
Second |
Early (non-expulsive) |
|
• Cervix fully dilated (10 cm)
• Presenting part of fetus reaches pelvic
floor
• Woman has the urge to push |
Second |
Late(expulsive) |
|
|
a
The third stage of labour begins with delivery
of the baby and ends with expulsion of
placenta.
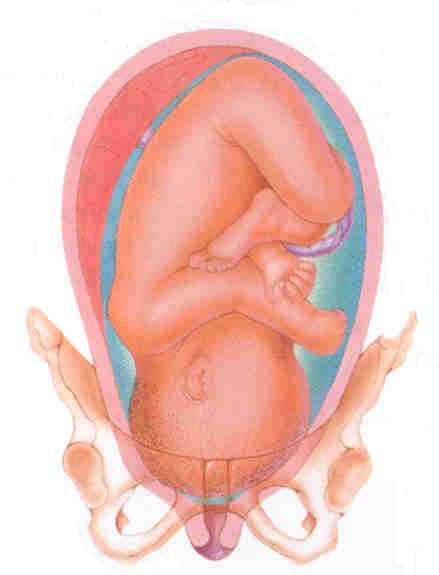
DESCENT
Abdominal palpation
• By abdominal palpation, assess descent in
terms of fifths of fetal head palpable above
the symphysis pubis (Fig
C-4 A�VD):
- A head that is entirely above the
symphysis pubis is five-fifths (5/5)
palpable
(Fig C-4 A�VB);
- A head that is entirely below the
symphysis pubis is zero-fifths (0/5)
palpable.
FIGURE C-4 Abdominal palpation for descent of
the fetal head
Vaginal examination
• If necessary, a vaginal examination may be
used to assess descent by relating the level
of the fetal presenting part to the ischial
spines of the maternal pelvis (Fig
C-5).
Note:
When there is a significant degree of caput
or moulding, assessment by abdominal
palpation using fifths of head palpable is
more useful than assessment by vaginal exam.
FIGURE C-5
Assessing descent of the fetal head by vaginal
examination; 0 station is at the level of the
ischial spine (Sp).
Presentation and position
Determine the presenting part
• The most common presenting part is the
vertex of the fetal head. If the vertex is
not the presenting part, manage as a
malpresentation (Table
S-12).
• If the vertex is the presenting part,
use landmarks on the fetal skull to determine
the position of the fetal head in relation to
the maternal pelvis (Fig
C-6).
FIGURE C-6 Landmarks of the fetal skull
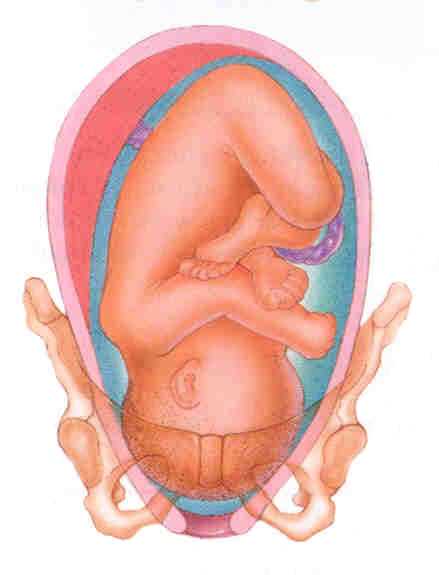
Determine the position of the fetal head
•
The fetal head normally engages in the
maternal pelvis in an occiput transverse
position, with the fetal occiput
transverse in the maternal pelvis (Fig
C-7).
FIGURE C-7
Occiput transverse positions
• With descent, the fetal head rotates so that
the fetal occiput is anterior in the maternal
pelvis (occiput
anterior positions, Fig C-8). Failure
of an occiput transverse position to rotate to
an occiput anterior position
should be managed as an occiput posterior
position.
FIGURE C-8
Occiput anterior positions
• An additional feature of a normal
presentation is a well-flexed vertex (Fig
C-9), with the occiput lower in the vagina
than the sinciput.
FIGURE C-9
Well-flexed vertex
Assessment of progress of labour
Once diagnosed, progress of labour is assessed
by:
• measuring changes in cervical effacement and
dilatation (Fig C-3
A�VE) during the latent phase;
• measuring the rate of cervical dilatation
and fetal descent (Fig
C-4, and Fig C-5)
during the active phase;
• assessing further fetal descent during the
second stage.
Progress of the first stage of labour should
be plotted on a partograph once the woman
enters the active phase of labour. A sample
partograph is shown in
Fig C-10.
Alternatively, plot a simple graph of cervical
dilatation (centimetres) on the vertical axis
against time (hours) on the horizontal axis.
Vaginal examinations
Vaginal examinations should be carried out at
least once every 4 hours during the first
stage of labour and after rupture of the
membranes. Plot the findings on a partograph.
• At each vaginal examination, record the
following:
- colour of amniotic fluid;
- cervical dilatation;
- descent (can also be assessed
abdominally).
• If the cervix is not dilated on first
examination it may not be possible to
diagnose labour.
- If contractions persist, re-examine
the woman after 4 hours for cervical
changes. At this stage, if there is
effacement and dilatation, the woman is
in labour; if there is no change, the
diagnosis is false labour.
• In the second stage of labour, perform
vaginal examinations once every hour.
�@
USING THE PARTOGRAPH
The WHO partograph has been modified to make
it simpler and easier to use. The latent phase
has been removed and plotting on the
partograph begins in the active phase when the
cervix is 4 cm dilated. A sample partograph is
included (Fig
C-10). Note that the partograph should be
enlarged to full size before use. Record the
following on the partograph:
Patient information:
Fill out name, gravida, para, hospital number,
date and time of admission and time of
ruptured membranes.
Fetal heart rate:
Record every half hour.
Amniotic fluid:
Record the colour of amniotic fluid at every
vaginal examination:
• I: membranes intact;
• C: membranes ruptured, clear fluid;
• M: meconium-stained fluid;
• B: blood-stained fluid.
Moulding:
• 1: sutures apposed;
• 2: sutures overlapped but reducible;
• 3: sutures overlapped and not reducible.
Cervical dilatation:
Assessed at every vaginal examination and
marked with a cross (X). Begin plotting
on the partograph at 4 cm.
Alert line:
A line starts at 4 cm of cervical dilatation
to the point of expected full dilatation at
the rate of 1 cm per hour.
Action line:
Parallel and 4 hours to the right of the alert
line.
Descent assessed by abdominal palpation:
Refers to the part of the head (divided into 5
parts) palpable above the symphysis pubis;
recorded as a circle (O) at every
vaginal examination. At 0/5, the sinciput (S)
is at the level of the symphysis pubis.
Hours:
Refers to the time elapsed since onset of
active phase of labour (observed or
extrapolated).
Time:
Record actual time.
Contractions:
Chart every half hour; palpate the number of
contractions in 10 minutes and their duration
in seconds.
• Less than 20 seconds:

• Between 20 and 40 seconds:

• More than 40 seconds:

Oxytocin:
Record the amount of oxytocin per volume IV
fluids in drops per minute every 30 minutes
when used.
Drugs given:
Record any additional drugs given.
Pulse:
Record every 30 minutes and mark with a dot
(��).
Blood pressure:
Record every 4 hours and mark with arrows.
Temperature:
Record every 2 hours.
Protein, acetone and volume:
Record every time urine is passed.
FIGURE C-10 The modified WHO Partograph
Figure C-11 is a sample partograph for
normal labour:
• A primigravida was admitted in the latent
phase of labour at 5 AM:
- fetal head 4/5 palpable;
- cervix dilated 2 cm;
- 3 contractions in 10 minutes, each lasting
20 seconds;
- normal maternal and fetal condition.
Note:
This information is not plotted on the
partograph.
• At 9 AM:
- fetal head is 3/5 palpable;
- cervix dilated 5 cm;
Note:
The woman was in the active phase of labour
and this information is plotted on the
partograph. Cervical dilatation is plotted
on the alert line.
- 4 contractions in 10 minutes, each lasting
40 seconds;
- cervical dilatation progressed at the rate
of 1 cm per hour.
• At 2 PM:
- fetal head is 0/5 palpable;
- cervix is fully dilated;
- 5 contractions in 10 minutes each lasting
40 seconds;
- spontaneous vaginal delivery occurred at
2:20 PM.
FIGURE C-11 Sample partograph for normal
labour
Progress of first stage of labour
• Findings suggestive of satisfactory
progress in first stage of labour are:
- regular contractions of progressively
increasing frequency and duration;
- rate of cervical dilatation at least 1 cm
per hour during the active phase of labour
(cervical dilatation on or to the left of
alert line);
- cervix well applied to the presenting
part.
• Findings suggestive of unsatisfactory
progress in first stage of labour are:
- irregular and infrequent contractions
after the latent phase;
- OR rate of cervical dilatation slower than
1 cm per hour during the active phase of
labour (cervical dilatation to the right of
alert line);
- OR cervix poorly applied to the presenting
part.
Unsatisfactory progress in labour can lead to
prolonged labour (Table
S-10).
Progress of second stage of labour
• Findings suggestive of satisfactory
progress in second stage of labour are:
- steady descent of fetus through birth
canal;
- onset of expulsive (pushing) phase.
• Findings suggestive of unsatisfactory
progress in second stage of labour are:
- lack of descent of fetus through birth
canal;
- failure of expulsion during the late
(expulsive) phase.
Progress of fetal condition
• If there are fetal heart rate
abnormalities (less than 100 or more than
180 beats per minute),
suspect fetal distress.
• Positions or presentations in labour other
than occiput anterior with a well-flexed
vertex are considered
malpositions or malpresentations.
• If unsatisfactory progress of labour
or prolonged labour is suspected,
manage the cause of slow progress.
Progress of maternal condition
Evaluate the woman for signs of distress:
• If the woman��s pulse is increasing,
she may be dehydrated or in pain.
Ensure adequate hydration via oral or IV
routes and provide adequate analgesia.
• If the woman��s blood pressure decreases,
suspect haemorrhage.
• If acetone is present in the woman��s
urine, suspect poor nutrition and give
dextrose IV.
NORMAL CHILDBIRTH
General methods of supportive care during
labour are most useful in helping the woman
tolerate labour pains
• Once the cervix is fully dilated and
the woman is in the expulsive phase of the
second stage, encourage the woman to
assume the position she prefers (Fig
C-12) and encourage her to push.
FIGURE C-12
Positions that a woman may adopt during
childbirth
Note:
Episiotomy is no longer recommended as a
routine procedure. There is no evidence that
routine episiotomy decreases perineal damage,
future vaginal prolapse or urinary
incontinence. In fact, routine episiotomy is
associated with an increase of third and
fourth degree tears and subsequent anal
sphincter muscle dysfunction.
Episiotomy
should be considered only in the case of:
• complicated vaginal delivery (breech,
shoulder dystocia, forceps, vacuum);
• scarring from female genital mutilation or
poorly healed third or fourth degree tears;
• fetal distress.
�@
Delivery of the head
• Ask the woman to pant or give only small
pushes with contractions as the baby��s head
delivers.
• To control birth of the head, place the
fingers of one hand against the baby��s head to
keep it flexed (bent).
• Continue to gently support the perineum as
the baby��s head delivers.
• Once the baby��s head delivers, ask the woman
not to push.
• Suction the baby��s mouth and nose.
• Feel around the baby��s neck for the
umbilical cord:
- If the cord is around the neck but is
loose, slip it over the baby��s head;
- If the cord is tight around the neck,
doubly clamp and cut it before unwinding it
from around the neck.
Completion of delivery
• Allow the baby��s head to turn spontaneously.
• After the head turns, place a hand on each
side of the baby��s head. Tell the woman to
push gently with the next contraction.
• Reduce tears by delivering one shoulder at a
time. Move the baby��s head posteriorly to
deliver the shoulder that is anterior.
Note:
If there is difficulty delivering the
shoulders,
suspect shoulder dystocia.
• Lift the baby��s head anteriorly to deliver
the shoulder that is posterior.
• Support the rest of the baby��s body with one
hand as it slides out.
• Place the baby on the mother��s abdomen.
Thoroughly dry the baby, wipe the eyes and
assess the baby��s breathing:
Note:
Most babies begin crying or breathing
spontaneously within 30 seconds of birth.
- If the baby is crying or breathing
(chest rising at least 30 times per minute)
leave the baby with the mother;
- If baby does not start breathing within
30 seconds, SHOUT FOR HELP and
take steps to resuscitate the baby.
Anticipate the need for resuscitation and have
a plan to get assistance for every baby but
especially if the mother has a history of
eclampsia, bleeding, prolonged or obstructed
labour, preterm birth or infection.
• Clamp and cut the umbilical cord.
• Ensure that the baby is kept warm and in
skin-to-skin contact on the mother��s chest.
Wrap the baby in a soft, dry cloth, cover with
a blanket and ensure the head is covered to
prevent heat loss.
• If the mother is not well, ask an
assistant to care for the baby.
• Palpate the abdomen to rule out the presence
of an additional baby(s) and proceed with
active management of the third stage.
ACTIVE MANAGEMENT OF THE THIRD STAGE
Active management of the third stage (active
delivery of the placenta) helps prevent
postpartum haemorrhage. Active management of
the third stage of labour includes:
• immediate oxytocin;
• controlled cord traction; and
• uterine massage.
Oxytocin
• Within 1 minute of delivery of the baby,
palpate the abdomen to rule out the presence
of an additional baby(s) and give oxytocin 10
units IM.
• Oxytocin is preferred because it is
effective 2 to 3 minutes after injection, has
minimal side effects and can be used in all
women. If oxytocin is not available,
give ergometrine 0.2 mg IM or prostaglandins.
Make sure there is no additional baby(s)
before giving these medications.
Do not give ergometrine to women with pre-eclampsia,
eclampsia or high blood pressure because it
increases the risk of convulsions and
cerebrovascular accidents.
Controlled cord traction
• Clamp the cord close to the perineum using
sponge forceps. Hold the clamped cord and the
end of forceps with one hand.
• Place the other hand just above the woman��s
pubic bone and stabilize the uterus by
applying counter traction during controlled
cord traction. This helps prevent inversion of
the uterus.
• Keep slight tension on the cord and await a
strong uterine contraction (2�V3 minutes).
• When the uterus becomes rounded or the
cord lengthens, very gently pull downward
on the cord to deliver the placenta. Do not
wait for a gush of blood before applying
traction on the cord. Continue to apply
counter traction to the uterus with the other
hand.
• If the placenta does not descend
during 30�V40 seconds of controlled cord
traction (i.e. there are no signs of placental
separation), do not continue to pull on the
cord:
- Gently hold the cord and wait until the
uterus is well contracted again. If
necessary, use a sponge forceps to clamp the
cord closer to the perineum as it lengthens;
- With the next contraction, repeat
controlled cord traction with counter
traction.
Never apply cord traction (pull) without
applying counter traction (push) above the
pubic bone with the other hand.
• As the placenta delivers, the thin membranes
can tear off. Hold the placenta in two hands
and gently turn it until the membranes are
twisted.
• Slowly pull to complete the delivery.
• If the membranes tear, gently examine
the upper vagina and cervix wearing high-level
disinfected gloves and use a sponge forceps to
remove any pieces of membrane that are
present.
• Look carefully at the placenta to be sure
none of it is missing. If a portion of the
maternal surface is missing or there are torn
membranes with vessels,
suspect retained placental fragments.
• If uterine inversion occurs,
reposition the uterus.
• If the cord is pulled off,
manual removal of the placenta may be
necessary.
Uterine massage
• Immediately massage the fundus of the uterus
through the woman��s abdomen until the uterus
is contracted.
• Repeat uterine massage every 15 minutes for
the first 2 hours.
• Ensure that the uterus does not become
relaxed (soft) after you stop uterine massage.
Examination for tears
•
Examine the woman carefully and repair any
tears to the cervix or
vagina or
repair episiotomy.
INITIAL CARE OF THE NEWBORN
• Check the baby��s breathing and colour every
5 minutes.
• If the baby becomes cyanotic (bluish)
or is having difficulty breathing (less
than 30 or more than 60 breaths per minute),
give oxygen by nasal catheter or prongs.
• Check warmth by feeling the baby��s feet
every 15 minutes:
- If the baby��s feet feel cold, check
axillary temperature;
- If the baby��s temperature is below
36.5�XC,
rewarm the baby.
• Check the cord for bleeding every 15
minutes. If the cord is bleeding, retie
cord more tightly.
• Apply antimicrobial drops (1% silver nitrate
solution or 2.5% povidone-iodine solution) or
ointment (1% tetracycline ointment) to the
baby��s eyes.
Note:
Povidone-iodine should not be confused with
tincture of iodine, which could cause
blindness if used.
• Wipe off any meconium or blood from skin.
• Encourage breastfeeding when the baby
appears ready (begins ��rooting��). Do not force
the baby to the breast.
Avoid separating mother from baby whenever
possible. Do not leave mother and baby
unattended at any time.
�@ |