|
Cesarean section (C-section) is the delivery of a newborn through
a surgical incision in the abdomen and front (anterior) wall of the
uterus. The C-section rate may approximate 30% in some hospitals,
particularly where high-risk pregnancies are managed. This rate of
C-section is usually less for women with uncomplicated
pregnancies.
Anatomy and Physiology
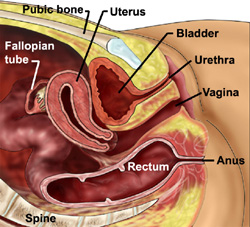
- The uterus or womb is a pear shaped organ that is found in the
pelvis at the top of the vagina. The uterus in a woman that is not
pregnant does not extend above the pubic bone (Figures 1, 2 and
3)
 |
 |
| Figure 1 - Anatomy of the uterus and
surrounding organs as seen in a section through the middle of
the body. |
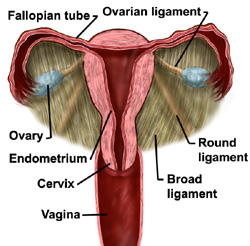
Figure 2 - Uterus as seen
from in front. |
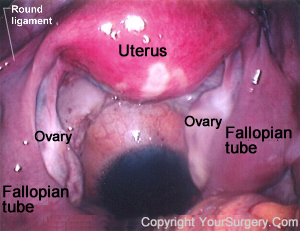 |
| Figure 3 - View of the uterus, ovaries, Fallopian tubes,
and round ligament through a laproscope. |
- In the pregnant woman at the end of pregnancy, the uterus
enlarges to approximately 40 centimeters (16 inches) above the
pubic bone
- The cervix is found at the lowermost portion of the uterus and
is the opening through which the fetus passes during delivery.
Normally, this opening is closed until late in the pregnancy
- Fertilization occurs within the fallopian tubes. The fallopian
tubes are found at the top of the uterus, one on each side. The
end of each fallopian tube has fingerlike projections called
fimbria which guide the egg from the ovary into the Fallopian tube
- The fertilized egg then passes from the Fallopian tube into
the cavity within the uterus where the fertilized egg implants
into the wall of the uterus. The site of implantation becomes the
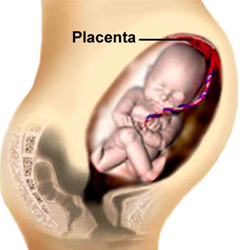
- As the egg develops into a fetus the remains attached to the
fetus through the umbilical cord. Thus the blood supply to the
fetus originates in the uterine wall
- The umbilical cord extends from the to the fetus where it
inserts at umbilicus (belly button) of the fetus
Reasons for the Increasing Rate of C-sections
- Greater emphasis on "quality survival" for the newborn, not
simply survival
- Continuous fetal monitoring
of heart rate increases the number of C-sections for fetal
distress
- More women are waiting to start childbearing until later in
life because of their careers. With advancing age of the mother
there is a greater risk of having other medical problems, thus the
C-section rate increases
- There has been a decrease in the number of forceps deliveries,
which in turn increases the number of C-sections
- Many obstetricians no longer wish to take the risk of a
vaginal breech (bottom first) delivery
- Women with prior a C-section often choose or are required to
have a repeat C-section
Indications for C-section
Some indications are controversial and some are accepted as the
standard.
- Fetal indications
- Abnormal fetal heart rate patterns (nonreassuring fetal
status) (Figure 4A)
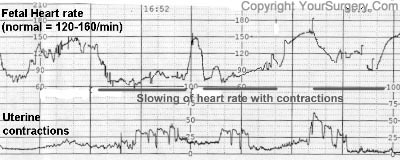 |
| Figure 4a - Non-reassuring fetal status - Printout
showing slowing of fetal heart rate with uterine
contractions, which led to cesarean section.
|
- Breech presentation of
the fetus ( bottom down instead of head down) (Figure 4B)
- Very low birth weight (<1500grams or 3.3 pounds)
- Active genital herpes lesions
- Idiopathic thrombocytopenia purpura - disease in which
there are low platelets in the blood and easy bleeding
- Major
malformations in the fetus making passage through the birth
canal difficult or impossible
 |
| Figure 4b - Breech presentation. Fetus
presents bottom side down
|
- Maternal indications
- Tumor obstructing the birth canal
- Large genital warts (condyloma)
- Cervical cerclage- a suture is placed in the cervix to
prevent preterm delivery. Cerclage may be permanent or temporary
to allow for vaginal delivery
- Certain vaginal surgeries (vaginal repair can break down)
- Conjoined
twins (Siamese twins)
- Prior surgery in which an incision was made in the uterus
(myomectomy -removal of fibroid tumor)
- HIV - The American College of Obstetricians and
Gynecologists recommends that HIV+ mothers should deliver the
fetus by C-section at 38 weeks of pregnancy to reduce the chance
of transmitting the virus to the fetus
- Maternal-Fetal Indications
- Cephalopelvic disproportion- either the baby is too large or
the pelvis is too small to allow passage
- Failure of the cervix to dilate or failure of the fetus to
pass down the birth canal
- Abruption - when the tears away from the uterus. This is an
emergency situation
- Previa - this is when the
implants over all or part of the cervix. (Figure 4C)
 |
| Figure 4C - previa. The is implanted over the
opening of the cervix thus preventing a vaginal delivery.
|
Making the Diagnosis
- Electronic fetal monitoring - monitoring of the fetus' heart
tracing. Repetitive decreases in heart rate may signal a decrease
in oxygen to the fetus (e.g. compression of the umbilical cord)
- Fetal scalp pH - monitors the acidity of the scalp tissue. An
elevated acidic reading (pH < 7.2) indicates a build up of
carbon dioxide and lactic acid in the blood, which occurs when the
fetus is poorly oxygenated
- Examination of the cervix -
- Rule out prolapse
of the umbilical cord
- Rule out bleeding from the cervix (e.g. with l previa
- Abdominal Ultrasound - ultrasound images of the uterus and its
contents are obtained
- Position of the fetus - head down or up
- Position of the relative to the cervix
- Size of the head (e.g. enlarged head due to hydrocephalus)
- Vaginal Ultrasound - similar to abdominal ultrasound but may
be more accurate in previa
- Test for HIV ?MRI - can be used to determine the position of
the fetus and
- Blood tests for Rh factor and bleeding tendency
The Procedure
- The skin is prepared with a solution that reduces the risk of
wound infection
- A catheter is placed in the bladder
- The hair near the incision may be shaved
- An incision is made in the skin
and is carried through the abdominal wall to enter the pelvis. The
skin incision may be made vertical (up and down) or transverse
(from side-to-side). The decision is based on many factors
including speed of entry, exposure needed, anticipated weight of
the baby and risk of wound infection. A transverse skin incision
is most common and is usually made 2-3 centimeters (one inch)
above the pubic bone (Figure A)
- The uterus is then identified. There is a layer of thin
tissue, which drapes over the anterior surface of the uterus and
then onto the bladder (the vesicouterine peritoneum). This layer
is incised so that the bladder can be retracted away form the
uterus to allow for the uterine incision. (Figure B) The incision
is then carried into the uterus to allow for delivery of the baby
- The uterine incision is then made down to the amniotic sack
(fetal membranes or bag of water). (Figure C)
- The uterine incision can be either transverse or vertical.
Ninety percent have a transverse uterine incision. Some
indications for a vertical incision in the uterus are a pre-term
fetus, a fetus that is not head down and with emergency
C-sections. Even in these situations a transverse incision may
sometimes be used. A woman that has a prior C-section with a
vertical uterine incision is usually not a candidate for vaginal
birth
- The fetal head or buttocks are then delivered through the
uterine incision followed by the rest of the body. (Figure D) Then
the is delivered
- Some obstetricians repair the uterus by first delivering the
uterus through the abdominal incision and some repair it while it
is still in the abdomen. The uterus is closed with one or two
layers of suture (Figure E)
- The layers of the abdominal wall are sutured and then the skin
closed with either suture or staples
Complications
- Injury to the bladder or ureters
- Bowel injuries may also occur. Risk factors are prior
abdominal surgery, and pelvic or abdominal infections, both of
which may lead to adhesions (scar tissue)
- Uterine atony. A condition in which the uterus does not
contract down adequately after delivery and lead to massive
hemorrhage. If conservative treatment fails, the surgeon may try
to tie off one or both of the arteries to the uterus. A
hysterectomy may be required on rare occasions to control the
bleeding if other measures fail
- Wound infection
- Urinary tract infection
- Failure of bowel function causing bowel distension
- Deep venous thrombosis. Blood clots in the veins of the legs
or pelvis that may go to the lungs (pulmonary embolus)
Care After Surgery
- Walking is important to prevent pneumonia and blood clots
- Diet initiallly consists of ice chips on the day of surgery,
fluids on the first day after surgery, and a regular diet two days
after surgery
- The catheter placed in the bladder at the time of surgery,is
usually removed the first day after surgery
- Fluids may be given in the vein up to and sometimes through
the first day after surgery
- Discharge to home may occur in two to five days depending on
the circumstances
Vaginal Birth After C-Section (VBAC)
Some women may be a candidate for vaginal birth after Cesarean
section
- Candidates for VBAC are
- One or two prior low transverse c-sections
- Clinically adequate pelvis (pelvis seems large enough based
on exam)
- Physician readily available throughout labor capable of
performing an emergency c-section.
- Available anesthesia and personnel for emergency
c-section
- There is a 60-80% success rate with VBAC. There is a higher
success rate when
- Prior c-section was performed for abnormal fetal heart tones
(nonreassuring fetal status)
- The woman has had at least one vaginal birth in the past
- Complications
- Uterine dehiscence at the old incision site. Women who have
dehiscence have a partial separation of their old incision and
may not need any repair if clinically stable
- Uterine rupture at the old incision site. The incidence of
rupture is 0.2-1.5%. Women with uterine rupture need an
emergency c-section
Procedures of Caesarean section
• Review for
indications. Ensure that vaginal delivery is not possible.
• Check for
fetal life by listening to the fetal heart rate and examine for
fetal presentation.
• Review
operative care principles.
• Use local
infiltration with lignocaine, ketamine, spinal anaesthesia or
general anaesthesia:
- Local
anaesthesia is a safe alternative to general, ketamine or spinal
anaesthesia when these anaesthetics or persons trained in their
use are not available;
- The use of
local anaesthesia for caesarean section requires that the provider
counsel the woman and reassure her throughout the procedure. The
provider should use instruments and handle tissue as gently as
possible, keeping in mind that the woman is awake and alert.
Note: In
the case of heart failure, use local infiltration anaesthesia with
conscious sedation. Avoid spinal anaesthesia.
• Start an IV
infusion.
• Determine if a
high vertical incision is indicated:
- an
inaccessible lower segment due to dense adhesions from previous
caesarean sections;
- transverse
lie (with babyˇ¦s back down) for which a lower uterine segment
incision cannot be safely performed;
- fetal
malformations (e.g. conjoined twins);
- large
fibroids over the lower segment;
- a highly
vascular lower segment due to placenta praevia;
- carcinoma of
the cervix.
• If the
babyˇ¦s head is deep down into the pelvis as in obstructed labour,
prepare the vagina for assisted caesarean delivery.
• Have the
operating table tilted to the left or place a pillow or folded linen
under the womanˇ¦s right lower back to decrease supine hypotension
syndrome.
OPENING THE ABDOMEN
• Make a midline vertical incision below the umbilicus to the pubic
hair, through the skin and to the level of the fascia (Fig P-19).
Note: If
the caesarean section is peformed under local anaesthesia,
make the midline incision that is about 4 cm longer than when
general anaesthesia is used. A Pfannenstiel
incision should
not be used as it takes longer, retraction is poorer and it
requires more local anaesthetic.
FIGURE P-19
Site of abdominal incision

ˇ@
• Make a 2ˇV3 cm
vertical incision in the fascia.
• Hold the
fascial edge with forceps and lengthen the incision up and down
using scissors.
• Use fingers or
scissors to separate the rectus muscles (abdominal wall muscles).
• Use fingers to
make an opening in the peritoneum near the umbilicus. Use scissors
to lengthen the incision up and down in order to see the entire
uterus. Carefully, to prevent bladder injury, use scissors to
separate layers and open the lower part of the peritoneum.
• Place a
bladder retractor over the pubic bone.
• Use forceps to
pick up the loose peritoneum covering the anterior surface of the
lower uterine segment and incise with scissors.
• Extend the
incision by placing the scissors between the uterus and the loose
serosa and cutting about 3 cm on each side in a transverse fashion.
• Use two
fingers to push the bladder downwards off of the lower uterine
segment. Replace the bladder retractor over the pubic bone and
bladder.
OPENING THE
UTERUS
• Use a scalpel
to make a 3 cm transverse incision in the lower segment of the
uterus. It should be about 1 cm below the level where the vesico-uterine
serosa was incised to bring the bladder down.
• Widen the
incision by placing a finger at each edge and gently pulling upwards
and laterally at the same time (Fig P-20).
• If the
lower uterine segment is thick and narrow, extend the incision
in a crescent shape, using scissors instead of fingers to avoid
extension of the uterine vessels.
It is important
to make the uterine incision big enough to deliver the head and body
of the baby without tearing the incision.
FIGURE P-20
Enlarging the uterine incision

ˇ@
DELIVERY OF
THE BABY AND PLACENTA
• To deliver the baby, place one hand inside the uterine cavity
between the uterus and the babyˇ¦s head.
• With the
fingers, grasp and flex the head.
• Gently lift
the babyˇ¦s head through the incision (Fig P-21), taking care not to
extend the incision down towards the cervix.
• With the other
hand, gently press on the abdomen over the top of the uterus to help
deliver the head.
• If the
babyˇ¦s head is deep down in the pelvis or vagina, ask an
assistant (wearing high-level disinfected gloves) to reach into the
vagina and push the babyˇ¦s head up through the vagina. Then lift and
deliver the head (Fig P-22).
FIGURE P-21
Delivering the babyˇ¦s head

FIGURE P-22 Delivering the deeply engaged head

• Suction the babyˇ¦s mouth and nose when delivered.
• Deliver the
shoulders and body.
• Give oxytocin
20 units in 1 L IV fluids (normal saline or Ringerˇ¦s lactate) at 60
drops per minute for 2 hours.
• Clamp and cut
the umbilical cord.
• Hand the baby
to the assistant for initial care.
• Give a single
dose of prophylactic antibiotics after the cord is clamped and cut:
- ampicillin 2
g IV;
- OR cefazolin
1 g IV.
• Keep gentle
traction on the cord and massage (rub) the uterus through the
abdomen.
• Deliver the
placenta and membranes.
CLOSING THE UTERINE INCISION
Note: If a Couvelaire uterus (swollen and discolored
by blood) is seen at caesarean section, close it in the normal
manner and observe.
• Grasp the
corners of the uterine incision with clamps.
• Grasp the
bottom edge of the incision with clamps. Make sure it is separate
from the bladder.
• Look carefully
for any extensions of the uterine incision.
• Repair the
incision and any extensions with a continuous locking stitch of 0
chromic catgut (or polyglycolic) suture (Fig P-23).
• If there is
any further bleeding from the incision site, close with
figure-of-eight sutures. There is no need for a routine second layer
of sutures in the uterine incision.
FIGURE P-23
Closing the uterine incision

CLOSING THE ABDOMEN
• Look carefully at the uterine incision before closing the abdomen.
Make sure there is no bleeding and the uterus is firm. Use a sponge
to remove any clots inside the abdomen.
• Examine
carefully for injuries to the bladder and repair any found.
• Close the
fascia with continuous 0 chromic catgut (or polyglycolic) suture.
Note:
There is no need to close the bladder peritoneum or the abdominal
peritoneum.
• If there
are signs of infection, pack the subcutaneous tissue with gauze
and place loose 0 catgut (or polyglycolic) sutures. Close the skin
with a delayed closure after the infection has cleared.
• If there are
no signs of infection, close the skin with vertical mattress
sutures of 3-0 nylon (or silk) and apply a sterile dressing.
• Gently push on
the abdomen over the uterus to remove clots from the uterus and
vagina.
PROBLEMS
DURING SURGERY
BLEEDING IS NOT CONTROLLED
• Massage the uterus.
• If the
uterus is atonic, continue to infuse oxytocin and give
ergometrine 0.2 mg IM and prostaglandins, if available. These drugs
can be given together or sequentially (Table S-8).
• Transfuse as
necessary.
• Have an
assistant press fingers over the aorta to reduce the bleeding until
the source of bleeding can be found and stopped.
• If bleeding
is not controlled, perform uterine and utero-ovarian artery
ligation or hysterectomy.
BABY IS BREECH
• If the baby is breech, grasp a foot and deliver it through
the incision.
• Complete the
delivery as in a vaginal breech delivery:
- Deliver the
legs and the body up to the shoulders, then deliver the arms;
- Flex (bend)
the head using the Mauriceau Smellie Veit manoeuvre.
BABY IS
TRANSVERSE
THE BABYˇ¦S
BACK IS UP
• If the back is up (near the top of the uterus), reach into
the uterus and find the babyˇ¦s ankles.
• Grasp the
ankles and pull gently through the incision to deliver the legs and
complete the delivery as for a breech baby.
THE
BABYˇ¦S BACK IS DOWN
• If the back is down, a high vertical uterine incision is
the preferred incision.
• After the
incision is made, reach into the uterus and find the feet. Pull them
through the incision and complete the delivery as for a breech
baby.
• To repair the
vertical incision, you will need several layers of suture.
ˇ@
PLACENTA
PRAEVIA
• If a low anterior placenta is encountered, incise through
it and deliver the fetus.
• After delivery
of the baby, if the placenta cannot be detached manually, the
diagnosis is placenta accreta, a common finding at the site of a
previous caesarean scar. Perform a hysterectomy.
• Women with
placenta praevia are at high risk of postpartum haemorrhage. If
there is bleeding at the placental site, under-run the
bleeding sites with chromic catgut (or polyglycolic) sutures.
• Watch for
bleeding in the immediate postpartum period and take appropriate
action.
ˇ@
POST-PROCEDURE CARE
• Review postoperative care principles.
• If bleeding
occurs:
- Massage the
uterus to expel blood and blood clots. Presence of blood clots
will inhibit effective uterine contractions;
- Give
oxytocin 20 units in 1 L IV fluids (normal saline or Ringerˇ¦s
lactate) at 60 drops per minute and ergometrine 0.2 mg IM and
prostaglandins (Table S-8). These drugs can be given together or
sequentially.
• If there
are signs of infection or the woman currently has fever,
give a combination of antibiotics until she is fever-free for 48
hours:
- ampicillin 2
g IV every 6 hours;
- PLUS
gentamicin 5 mg/kg body weight IV every 24 hours;
- PLUS
metronidazole 500 mg IV every 8 hours.
• Give
appropriate analgesic drugs.
HIGH VERTICAL (ˇ§CLASSICALˇ¨) INCISION
• Open the abdomen through a midline incision skirting the
umbilicus. Approximately one-third of the incision should be above
the umbilicus and two-thirds below.
• Use a scalpel
to make the incision:
- Check the
position of the round ligaments and ensure that the incision is in
the midline (the uterus may have twisted to one side);
- Make the
uterine incision in the midline over the fundus of the uterus;
- The incision
should be approximately 12ˇV15 cm in length and the lower limit
should not extend to the utero-vesical fold of the peritoneum.
• Ask an
assistant (wearing high-level disinfected gloves) to apply pressure
on the cut edges to control the bleeding.
• Cut down to
the level of the membranes and then extend the incision using
scissors.
• After
rupturing the membranes, grasp the babyˇ¦s foot and deliver the baby.
• Deliver the
placenta and membranes.
• Grasp the
edges of the incision with Allis or Green Armytage forceps.
• Close the
incision using at least three layers of suture:
- Close the
first layer closest to the cavity but avoiding the decidua with a
continuous 0 chromic catgut (or polyglycolic) suture;
- Close the
second layer of uterine muscle using interrupted 1 chromic catgut
(or polyglycolic) sutures;
- Close the
superficial fibres and the serosa using a continuous 0 chromic
catgut (or polyglycolic) suture with an atraumatic needle.
• Close the
abdomen as for lower segment caesarean section (page P-48).
The woman should
not labour with future pregnancies.
TUBAL LIGATION AT CAESAREAN
Tubal ligation can be done immediately following caesarean section
if the woman requested the procedure before labour began
(during prenatal visits). Adequate counselling and informed
decision-making and consent must precede voluntary sterilization
procedures; this is often not possible during labour and delivery.
• Review for
consent of patient.
• Grasp the
least vascular, middle portion of the fallopian tube with a Babcock
or Allis forceps.
• Hold up a loop
of tube 2.5 cm in length (Fig P-24 A).
• Crush the base
of the loop with artery forceps and ligate it with 0 plain catgut
suture (Fig P-24 B).
• Excise the
loop (a segment 1 cm in length) through the crushed area (Fig P-24).
• Repeat the
procedure on the other side.
FIGURE P-24
Tubal ligation

ˇ@
ˇ@ |